Background: During the COVID-19 pandemic, studies have shown a possible association between dementia and adverse outcomes, with mortality rates reportedly as high as 2.4 times greater than compared to patients without dementia. Despite these preliminary findings, the relationship has not been conclusively established. Management of patients with dementia is complex, including a higher risk of delirium. This study intends to elucidate the burden of comorbid complications between individuals with dementia who are hospitalized for COVID-19, compared to their non-dementia counterparts.
Methods: A retrospective analysis using the 2020 National Inpatient Sample of 816,960 COVID-19-positive patients aged >64 years with 180,845 (22.1%) with dementia was conducted. Multivariate regression analysis and propensity score-matched analysis were performed to compare in-hospital mortality, comorbidity rates, hospitalization charges, length of stay, and disposition statuses between the two groups.
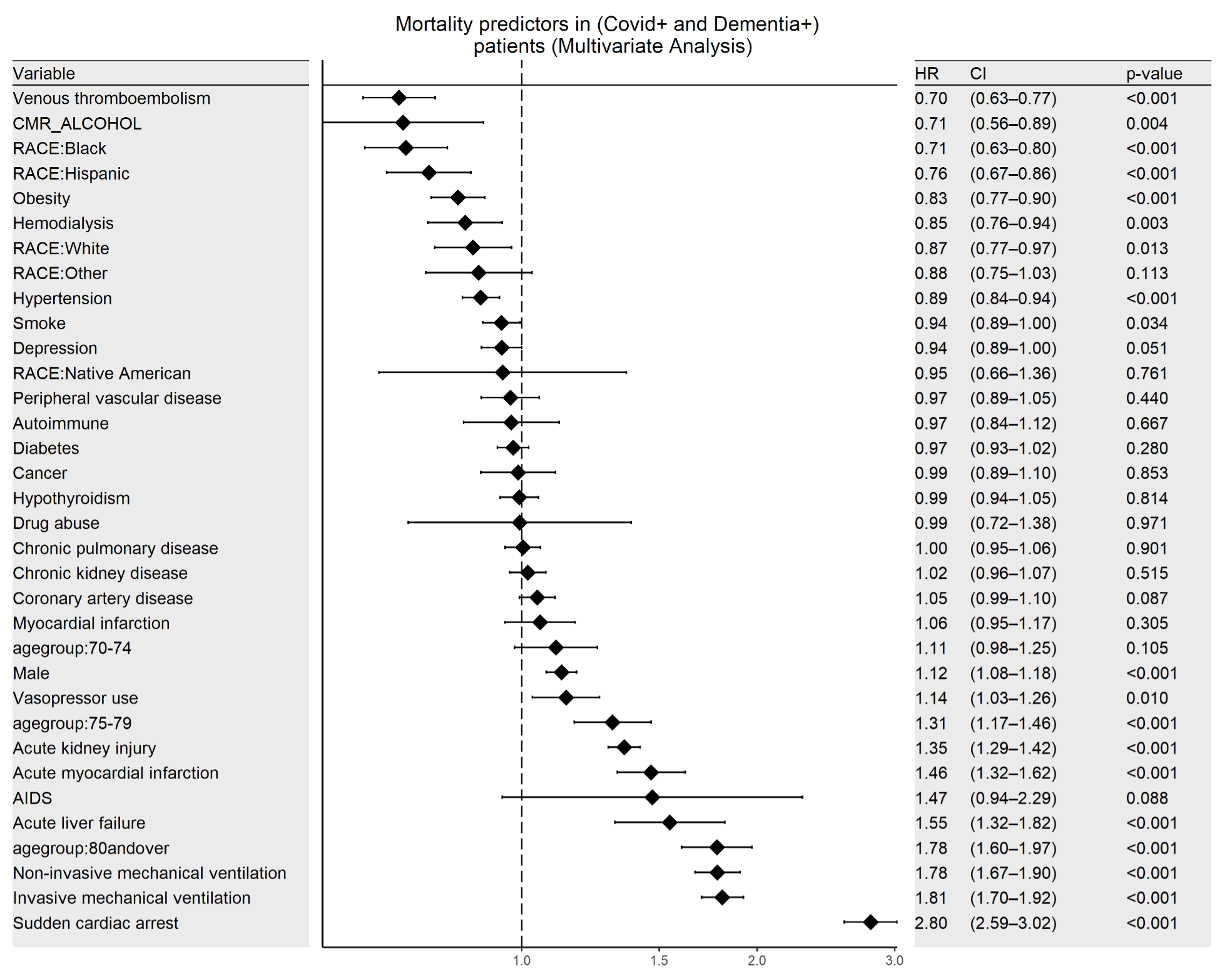
Results: Among the 361,690 COVID-19 and dementia patients, the odds ratio for in-hospital mortality is 1.16 (95% CI 1.12-1.2). Patients with dementia experience a higher adjusted odds ratio for acute kidney injury (aOR 1.21). However, patients with dementia did not differ significantly in acute liver failure (aOR 0.68), sudden cardiac arrest (aOR 0.88), vasopressor use (aOR 0.80), venous thrombi embolism (aOR 0.89), hemodialysis (aOR 0.66), invasive or non-invasive mechanical ventilation (aOR 0.68 and aOR 0.77 respectively), stroke, (aOR 0.95) and acute myocardial infarction (aOR 0.95). Individuals with COVID-19 and dementia did have a higher disposition to another facility (50.6% vs 27.9%) compared to the routine care follow-up of individuals without dementia (37.7% vs 9.9%). The adjusted mean length of stay was 0.64 days higher for COVID-19 patients with dementia but the mean total hospitalization cost for $6075.2 lower.
Conclusions: Our analysis underscores the nuanced interplay between dementia and COVID-19, marking a dichotomy in patient outcomes. Patients with both COVID-19 and dementia demonstrated an increased risk of in-hospital mortality and acute kidney injury, while other complications remained statistically similar to non-dementia counterparts. Furthermore, dementia patients frequently require transfer to secondary care facilities, implying greater post-hospital care requirements. Surprisingly, despite a marginally longer stay, hospitalization costs for dementia patients were lower. Clinicians managing older adults with COVID-19 and dementia must exercise heightened vigilance for mortality risk and acute kidney injury while care coordinators should prepare for enhanced post-discharge needs. However, the lack of statistically significant prevalence of most comorbid complications suggests that a more targeted, dementia-specific approach to patient management may not be required.