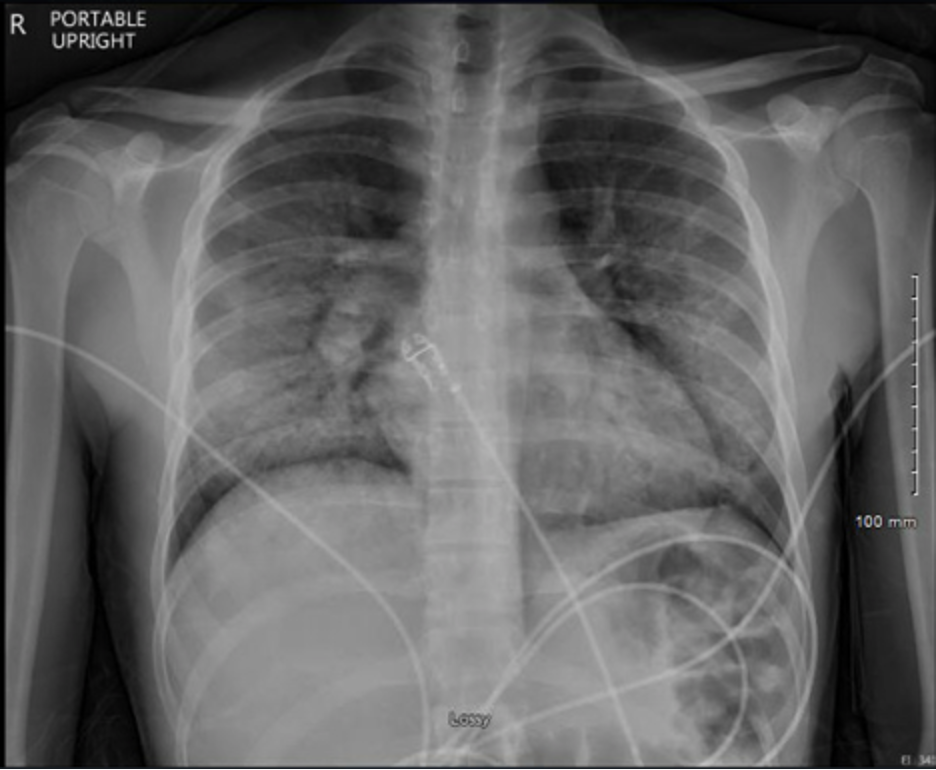
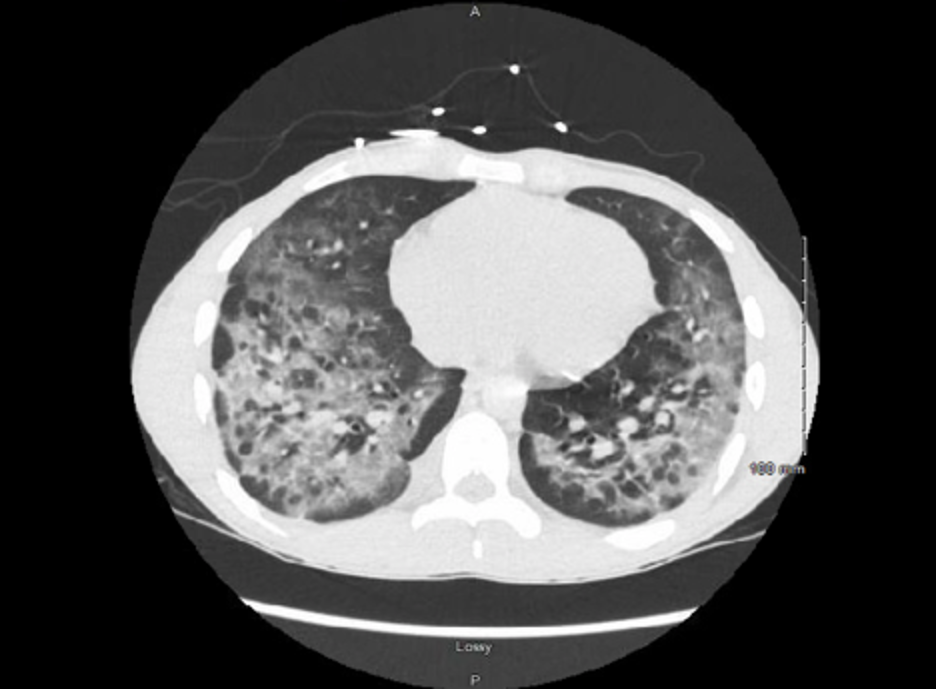
Case Presentation: A previously healthy, 20-year-old Caucasian male presented with worsening dyspnea after being diagnosed with pneumonia a week ago, and failed outpatient treatment with azithromycin. He denied sick contacts or recent travel; he endorsed vaping nicotine and THC oil once a week socially. On presentation, he was febrile to 100.8F, tachypneic to RR of 40, and required 4L of O2 on an oxygen mask. He tested negative for COVID-19 one week prior to presentation; however, initial CXR demonstrated diffuse bilateral airspace interstitial opacity, and the inflammatory markers, such as ferritin, LDH, CRP were elevated, which was concerning for possible false-negative COVID-19 infection. He also had leukocytosis and elevated procalcitonin, which are suggestive of possible CAP, and he was started on ceftriaxone. Eosinophilia present on admission and considered ANCA vasculitis as a possible differential diagnosis. The AHRF got worse, needed optiflow 35% O2, and 40% FiO2, and he was started on methylprednisolone overnight per MICU fellow’s suggestion. ID and Pulmonary were consulted, and he underwent chest CT, which demonstrated bilateral ground-glass opacities, and BAL and transbronchial biopsy–negative COVID, extended viral NAAT, and cytology. The remaining labs from the initial workup: sputum culture, blood cultures, COVID antibody, Flu NAAT, serum IgE, urine antigens for Legionella, Histoplasma, Blastomyces, Aspergillus, Mycoplasma NAAT, Chlamydia NAAT, Quantiferon gold test, HIV, ANA, p-ANCA, and c-ANCA all came back negative. He was diagnosed with e-cigarette/vaping-associated lung injury (EVALI) as a diagnosis of exclusion and continued on methylprednisolone. He was hospitalized for 7 days total and went home on oxygen. He was off oxygen on a pulmonary follow-up appointment and has been continuing prednisone taper.
Discussion: The prevalence of vaping has significantly increased among teenagers and young adults. As of 2020, 2807 cases of EVALI have been reported to the CDC. Among these reported cases, 66% were male, and 37% of patients were 18 to 24 years old. Typical presentations for EVALI include fever, non-productive cough, dyspnea, leukocytosis which would usually indicate possible CAP. It is important for clinicians to consider EVALI by obtaining a thorough social history regarding vaping use in the last 6 weeks, especially when young patients fail to improve after initiating antibiotic therapy. The exact cause of EVALI is not known, but possible causes include vitamin E acetate as well as those that contain vape juices with THC. Due to the rapid decline in respiratory failure, it is important to start corticosteroid treatment early. Radiographic imaging typically reveals a bilateral ground-glass opacification, which has also been demonstrated in COVID-19 infection. Some specific findings of Chest CT abnormalities in COVID-19 are often bilateral, have a peripheral distribution, and involve the lower lobes. Infectious workup usually will be unrevealing, and while BAL is not necessary to confirm EVALI, it may help to rule out other infectious causes.
Conclusions: As the prevalence of EVALI continues to rise, clinicians should have a high suspicion of EVALI in patients who present with dyspnea and negative infectious workup. Administration of corticosteroids has shown remarkable efficacy in improving dyspnea; however, many patients may have chronic lung injury and may require oxygen long term. Cases of EVALI should continue to be reported in order to better monitor the trend of the disease.