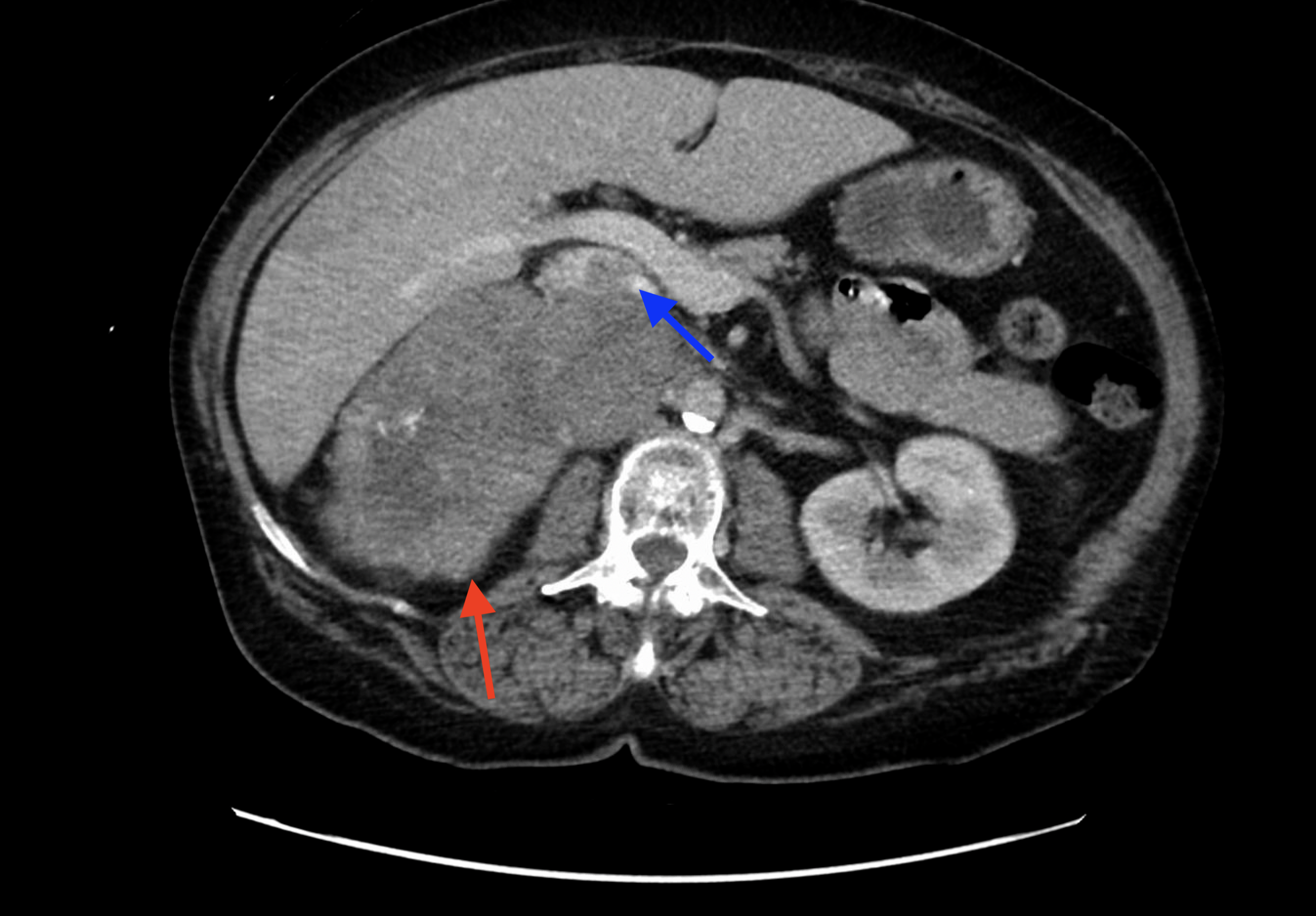
Case Presentation: A 59-year-old female presented with a one-month history of right upper quadrant abdominal pain and unexplained weight loss. On initial examination, the patient had a BMI of 27.1 kg/m2, blood pressure of 134/88 mmHg. A computerized tomography (CT) scan revealed a substantial tumor centered in the right adrenal gland region, compressing the inferior margin of the liver and extends into the intrahepatic inferior vena cava (Figure 1). Sonographic study showed invasion into the right atrium (Figure 2). Extensive hormonal studies showed an excess in both cortisol and androgen, as evidenced by elevated free cortisol level, elevated dehydroepiandrosterone sulfate level, and elevated total testosterone level. Primary aldosteronism and pheochromocytomas were ruled out as plasma renin activities, plasma aldosterone, plasma fractionated free metanephrine, and fractionated urine metanephrine levels were all within the normal range.The tumor’s size, radiographic features, and biochemical profile of combined glucocorticoid and androgen excess strongly suggested of adrenocortical carcinoma (ACC). Due to the tumor’s significant inferior vena caval and hepatic invasion, it was deemed unresectable for curative treatment. A percutaneously CT-guided biopsy was performed, and pathological examination revealed adrenal cortical neoplasm with extensive necrosis, confirming the diagnosis of ACC. Palliative treatment option with mitotane and immunotherapy was offered, but the patient declined this option and opted for comfort-focused care.
Discussion: The advancement and increased accessibility of imaging technology has led to a rise in detection of incidental adrenal findings. While most of these adrenal masses consist of small, benign, and non-functional adrenocortical adenomas, further evaluation to characterize the functional status and malignant potential of these masses is important to ensure early detection of malignant causes such as metastases, sarcomas, lymphomas, and ACC. The first step is to investigate the adrenal mass’ hormonal activity for cortisol, aldosterone, and catecholamine secretion. Assessment for potential malignant causes involves analyzing radiographic features of adrenal masses. Larger than 4cm, heterogenous, and rapidly growing tumors are correlated with malignancy. ACC is a rare form of highly aggressive malignant adrenal tumor often associated with signs and symptoms of hormonal excess. ACC accounts for 0.3% of all adrenal tumors with an annual incidence of 0.7-2 cases per million individuals and a 5-year mortality rate of 75% to 90%. The diagnosis of ACC relies on radiographic features, biochemical profiles, and exclusion of benign causes. When the suspicion for ACC is high, surgical resection should be strongly considered for diagnosis, prognostication, and treatment. Adrenal percutaneous biopsy is an option for diagnosis, though non-invasive diagnosis is preferrable to minimize the risk of needle track seeding. Pheochromocytomas must be thoroughly worked up and excluded prior to percutaneous biopsy to avoid eliciting an adrenal hypertensive crisis. Surgical resection remains the primary curative treatment. Debulking surgery and systemic therapy with mitotane may be done for palliative intent.
Conclusions: Given the complexity of ACC, multidisciplinary discussions among oncologists, surgeons, radiologists, endocrinologists, and pathologists are vital in determining appropriate diagnostic steps and management plan for each patient.