Background: Physician communication scores within the HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) directly impacts a hospitals STAR rating. Provider engagement is essential in improving clinical outcomes, quality of care and overall efficiency. There is a high rate of physician burnout and disengagement post pandemic. When physicians are disengaged the hospitals do not prosper. The hospitalist medicine team at our organization discharges over 10,000 patients a year, in 2021 there was a significant downward trend in physician communication scores, further impacting physician frustration and disengagement. Physicians believed the survey results were not a true representation of their role in the patients care and they desired real time feedback on their performance.
Purpose: Creating a sustainable strategy that increases provider engagement and in turn improves the quality and efficiency of care we provide our patients, ultimately improving patient experience. Overall goal of improving physician communication scores in the HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems through a real time operational feedback communication loop.
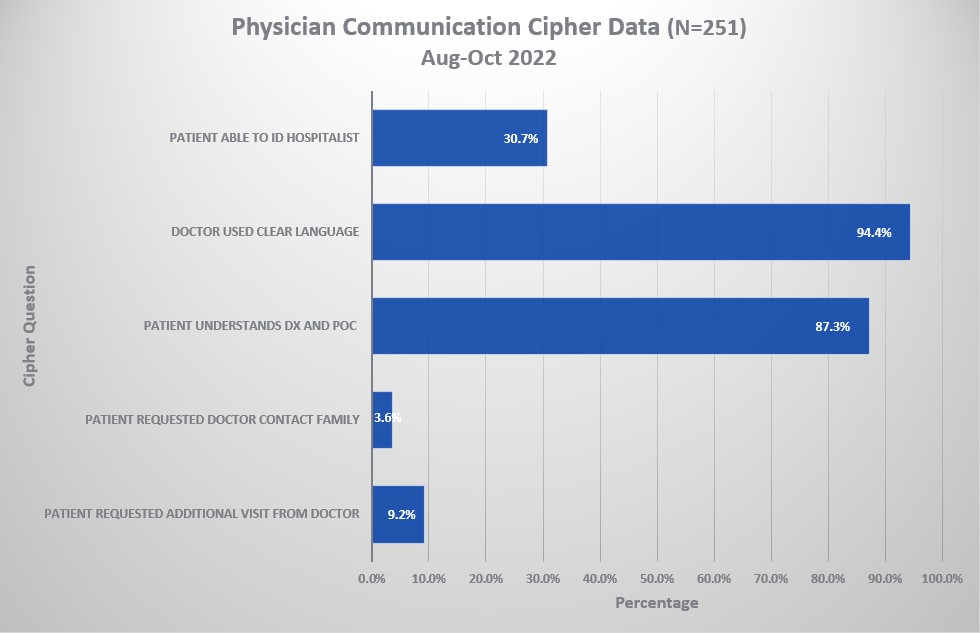
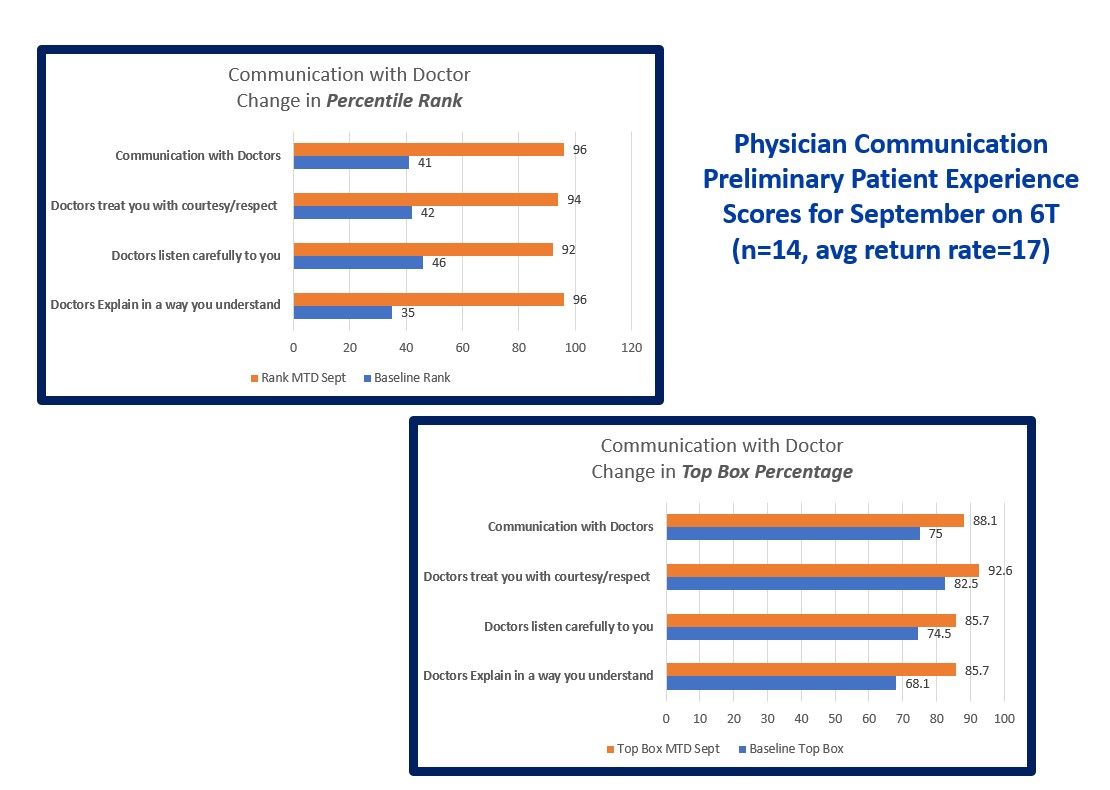
Description: Review of the current physician communication processes on one geographic unit was conducted. Opportunities for improvement were identified. The focus was on the 3 physician communication questions in the HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems). The aim was to improve patient recognition of the attending physician and to ensure they understood the feedback they provided on the survey pertained to that attending coordinating their care. A real time operational feedback loop communication between the patient and the provider was created through a script created in an analytic tool. Patients were asked the name of the provider in charge of their care, if they understood their diagnosis and plan of care, and were asked if they required further explanation from their physician. During this communication the patient was reoriented to the doctor in charge of their care and the feedback received from the patient went directly to the provider in real time. Data was compiled for a two month period (N=251 patient’s interviewed), results revealed that the doctor used clear language 94% of the time, patients understood their diagnosis and plan of care 87% of the time and only 30% of patients were able to identify their physician. Preliminary patient satisfaction data for physician communication for the following month was drastically improved from the 41st percentile rank to the 96th percentile rank.
Conclusions: Utilization of a real time operational feedback communication loop enhanced the ability for the provider to recognize the opportunity to improve communication with their patients. Provider engagement leads to improved quality outcomes and improved patient satisfaction.