Background: The year 2020 was pivotal for physician trainees. The harrowing disparities in SARS-CoV-2 infection and deaths left many trainees with a sense of anguish and urgency for working towards health equity. However, surveys of Internal Medicine residents have shown that their knowledge of healthcare disparities is poor, with minimal improvement and exposure during training. More informed providers may help reduce healthcare disparities. To address this need, we created the Stanford Internal Medicine Health Equity, Advocacy and Research program (Stanford IM HEARs).
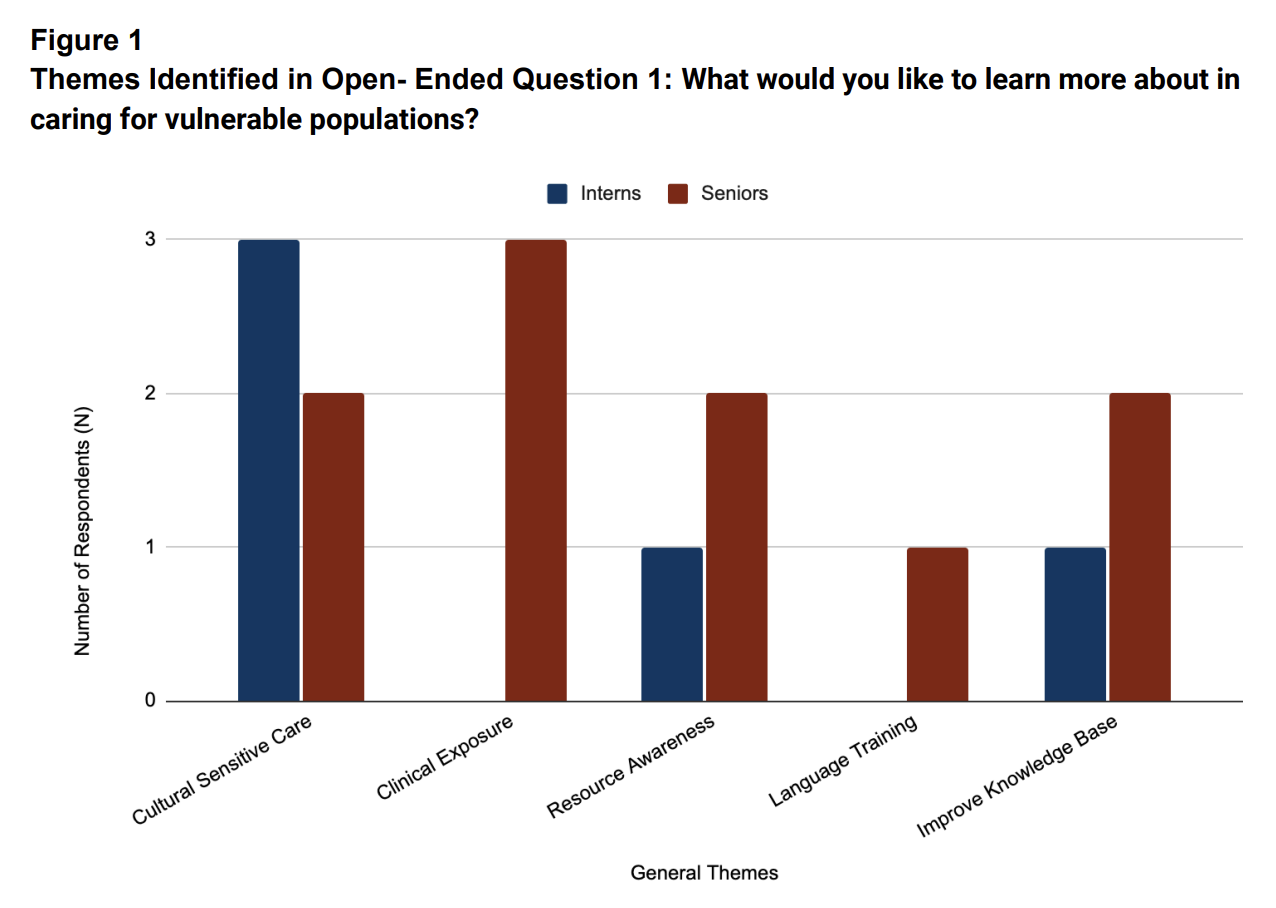
Purpose: To address the need for physician leaders to champion health equity work, Stanford IM HEARs was formed. Two Stanford residents worked with residency leadership to form the initial core working group of the program. A needs assessment survey was created and circulated to categorical residents and data were collected from residents interested in having a career focused on health equity.
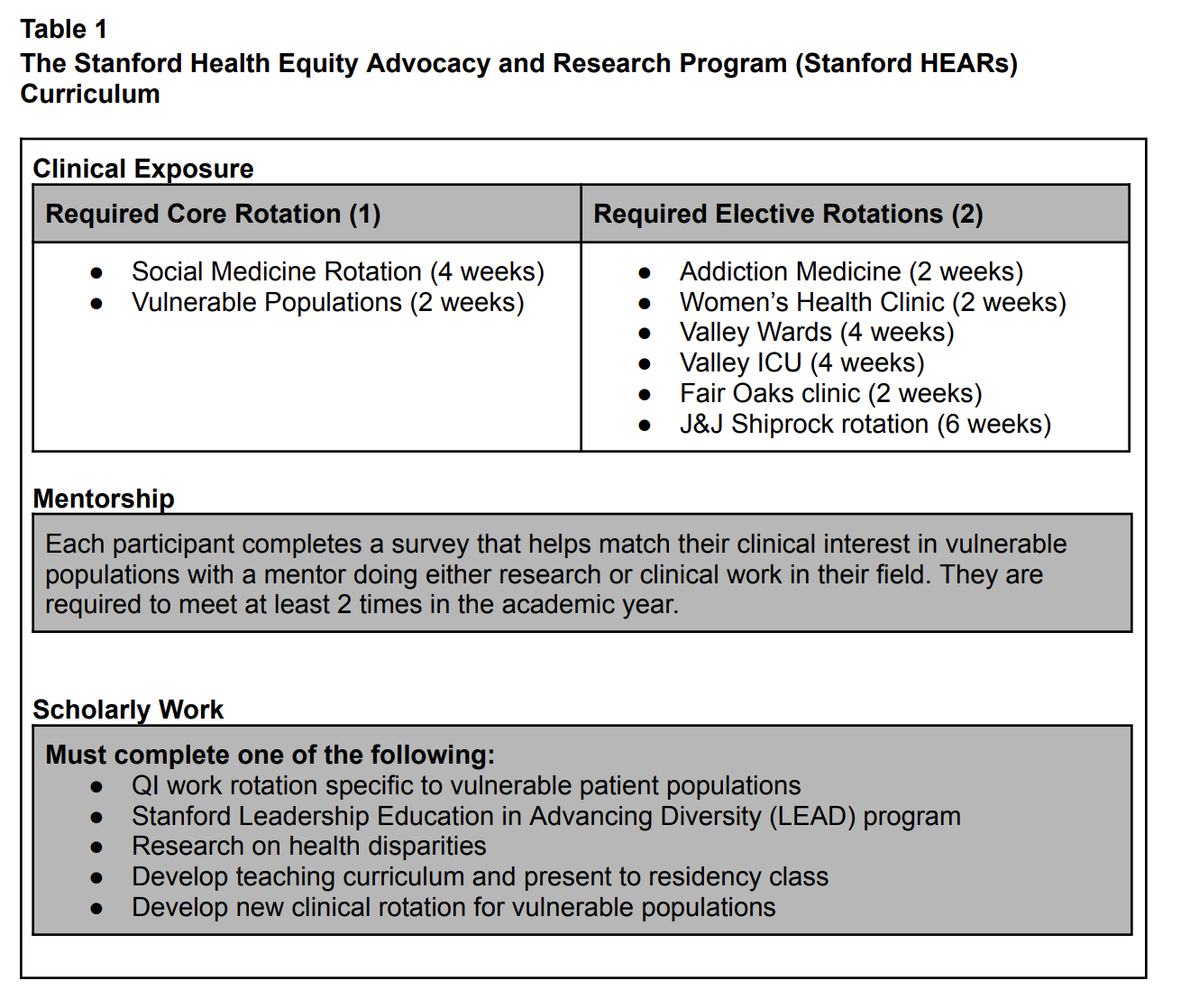
Description: Findings and program results: In 2020, 15 out of 119 categorical residents expressed interest in careers focused on local underserved patient populations and were asked to complete the survey. A total of 87% of respondents felt that residency training in caring for underserved patient populations was extremely important, but only 7% felt extremely comfortable in their knowledge and ability to provide care for vulnerable populations. Qualitative data from the surveys was used to design the HEARs program in 2021. The components include: (1) dedicated clinical rotations caring for marginalized patients, (2) pairing of residents with mentors, (3) completion of a scholarly project and, (4) a 2-week capstone course with experts in community health, health equity and advocacy. Since 2021-2023, 28 residents have joined the HEARs program resulting in quality improvement projects, research and medical education programs to promote equity in the hospital and creation of new community partnerships between Stanford and community-based groups. Interest in the program has grown exponentially from 3 members in 2020 to an incoming class of 19 participants for this academic year.
Conclusions: A needs survey resulted in creation of dedicated training in the care of underserved patients during residency. Rapid growth of interest results in an ability to include community partners in care delivery and strategies to reduce disparities. Our findings may serve to inform similar programs including those for hospital physicians who desire to contribute to health equity.