Background: Many cancer centers use the hospitalist model in the inpatient setting (1) since hospitalists provide high quality, cost efficient care (2). Our 678-bed quaternary hospital uses oncology hospitalist teams to care for all inpatients with solid tumor malignancies with medical oncology and palliative care consulting as needed. Internal medicine residents and advanced practice fellows rotate in two-week blocks on the oncology hospitalist teams and we created a curriculum for trainees that focuses on inpatient management of people with advanced solid tumors.
Purpose: The purpose of our curriculum was to complement bedside teaching with structured didactics given by medical oncologists, oncology hospitalists, and clinical pharmacists over a two-week block.
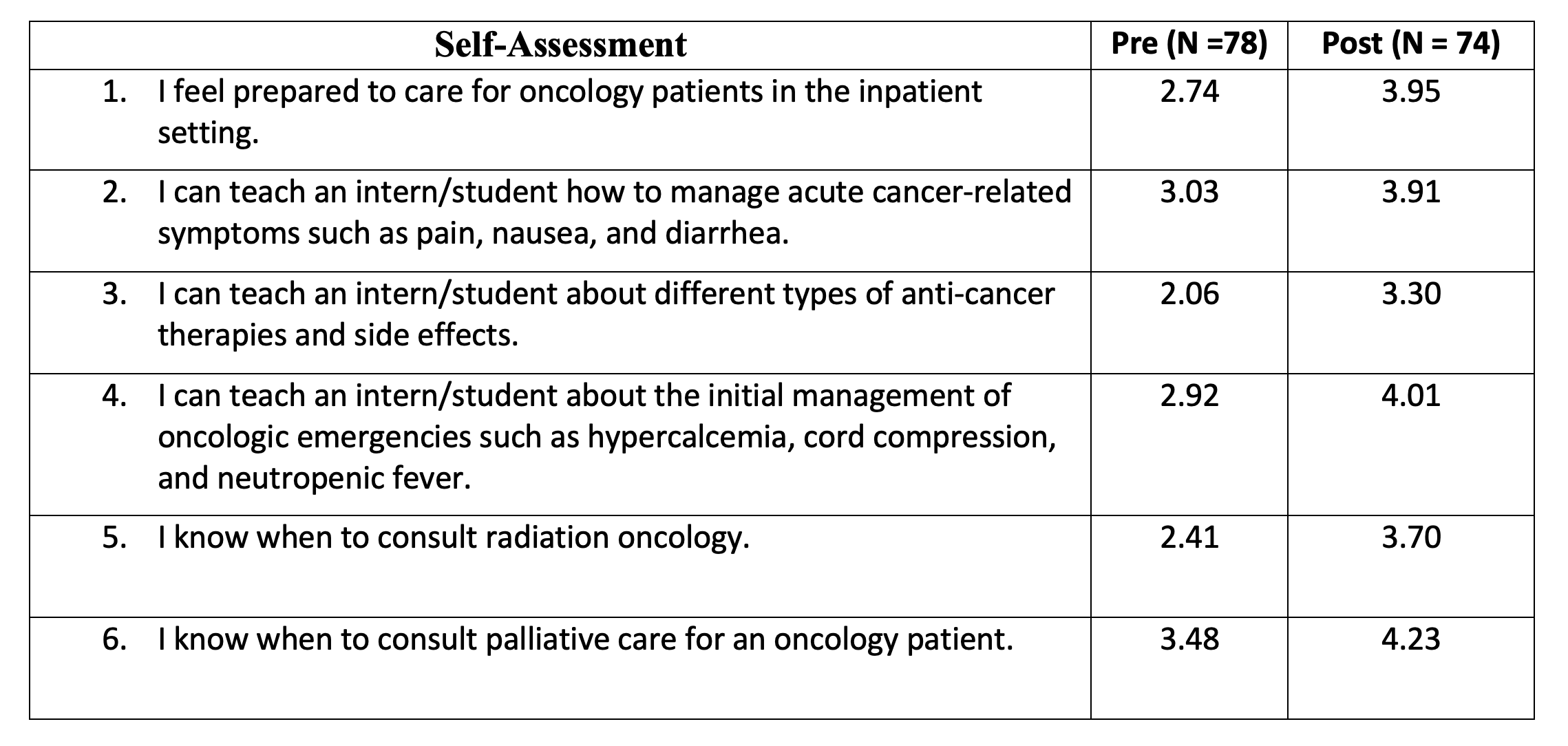
Description: The oncology hospitalist teaching service consists of two teams, each comprised of an attending, an advanced practice provider, and a trainee. Team 1 has a second- or third-year internal medicine resident, and Team 2 has an advanced practice fellow–an ACNP or PA who is enrolled in a 13-month hospital medicine fellowship program. On rare occasions, medical students also rotate through the oncology service. The average daily team census is 12 patients with a cap of 14. Rounds use the “discovery” model in which the entire team rounds on the patients together and the trainee leads bedside discussions with the patient. This model improves rounding efficiency, streamlines consistency in communication of complex information, and permits direct observation of bedside communication and physical exam skills. In addition to bedside teaching, trainees receive five core inpatient didactics: 1. Advanced symptom management: pain, nausea, vomiting, diarrhea, and constipation2. Common cancer-directed therapies and clinically important toxicities3. Oncologic emergencies4. Palliative procedures5. Work up of a new solid tumor diagnosis6. Introduction to radiation oncologyThe didactics are 30-minute interactive lectures that are given three days per week by inpatient clinical pharmacists, oncology fellows, and oncology hospitalist faculty. Learners are given pre- and post-rotation surveys, asking to self-rate their skills and knowledge on a 5-point Likert scale from 1 (strongly disagree) to 5 (strongly agree). Results from July 1, 2020, to June 30, 2022, are shown in Figure 1.
Conclusions: As hospital medicine expands into more specialized care, a curated curriculum can increase learner engagement and confidence. This innovation is unique in that it encourages multidisciplinary collaboration to accomplish educational objectives.