Background: Montefiore Health System (MHS) rapidly expanded from three hospitals in close proximity to eleven hospitals across hundreds of miles. The structure of the new health system follows a hub and spoke model with the concentration of specialty care located at the hub which is the Moses campus in Bronx, NY. In order to best serve all patients within the health system a new transfer center and transfer process was required. In addition to geography, the transfer process is challenged by non-communicating electronic health records. In order to facilitate care for patients across the health system a quality improvement project focusing on transfers into the medicine service at the core hospital was undertaken.
Purpose: The aim of the quality improvement project was multi-tiered. We sought improve the process of transfer acceptance by making it faster and easier for sending hospitals. We also wanted to increase our volume of transfers to the flagship hospital of the Montefiore Health System. Lastly, our goal was to build trust and strengthen the relationships of all of the hospitals within the health system.
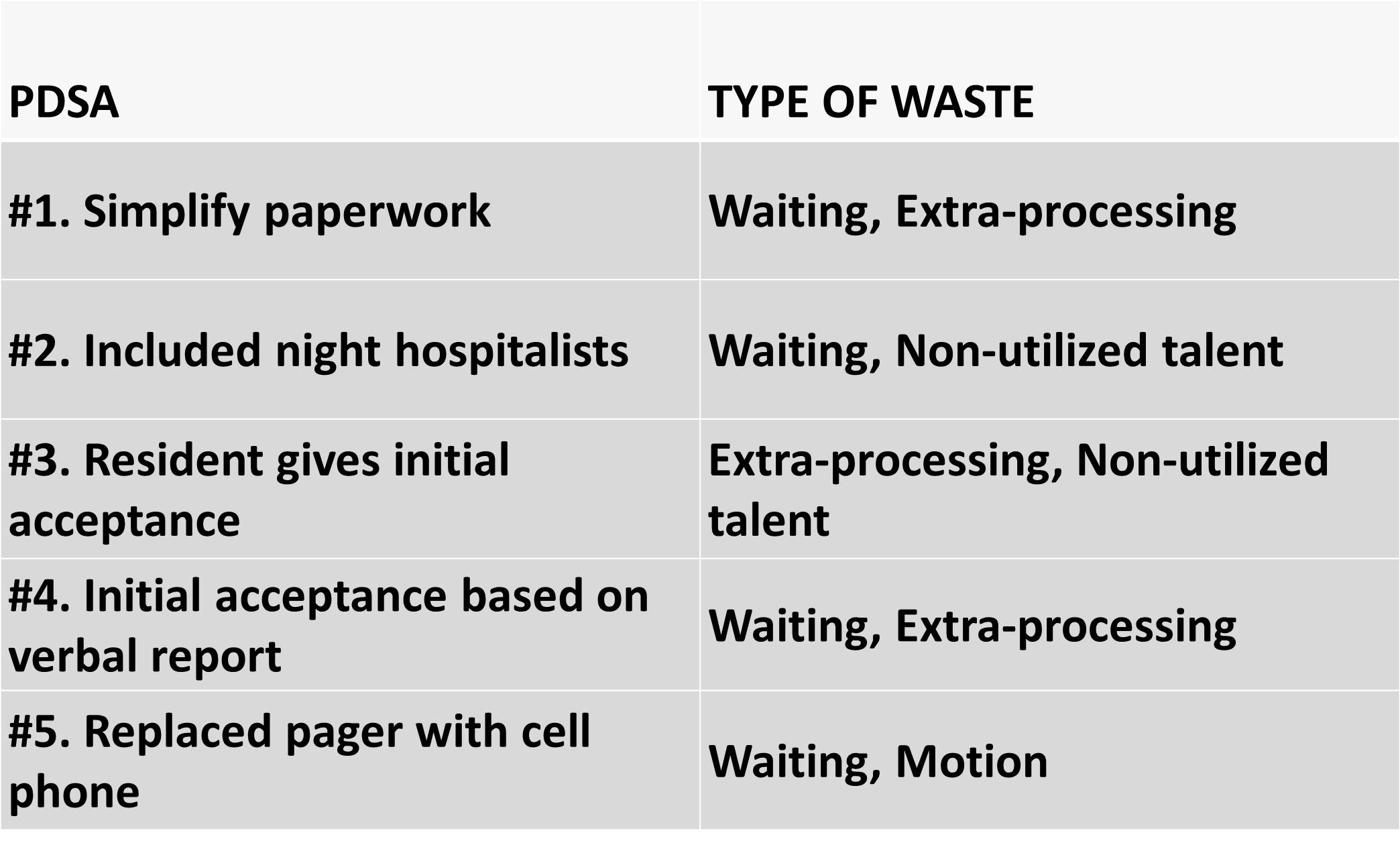
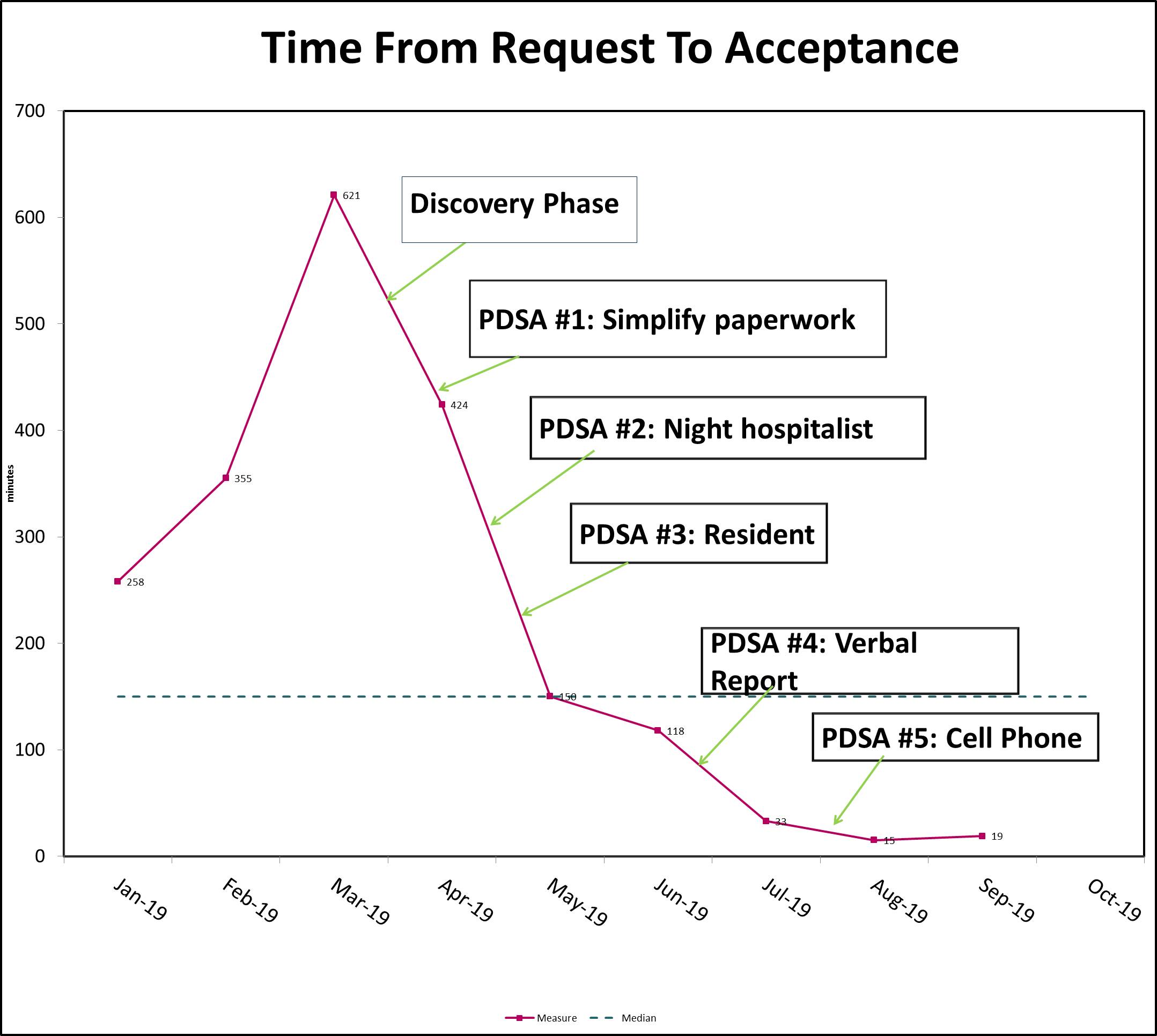
Description: The medicine transfer process was developed over a 10 month time period from January 2019 to October 2019. Using Quality Improvement methodology the transfer process was revamped to identify and eliminate waste. A multi-disciplinary team was formed including the medical service director, medicine attendings, transfer center director and transfer center staff members. A discovery phase included visiting multiple satellite hospitals and interviews with physicians and operational leaders. The multi-disciplinary team identified the time from transfer request to transfer acceptance as a key driver of volume of transfer requests and ultimately volume of transfers. A total of 5 interventions (PDSA cycles) were implemented to eliminate various types of waste (Figure 1). The time from transfer request to acceptance decreased from a peak of 10 hours to a sustained performance of less than one hour. The transfer volume to the Medicine service nearly doubled from 260 transfers in 2018 to 470 transfers in 2019.
Conclusions: This quality improvement project used PDSA cycles to improve the time from transfer request to acceptance at the flagship hospital at a large health system. Next steps include introducing the Medicine transfer process to other clinical services at the flagship location and reviewing the experiences of the teams who receive transferred patients.