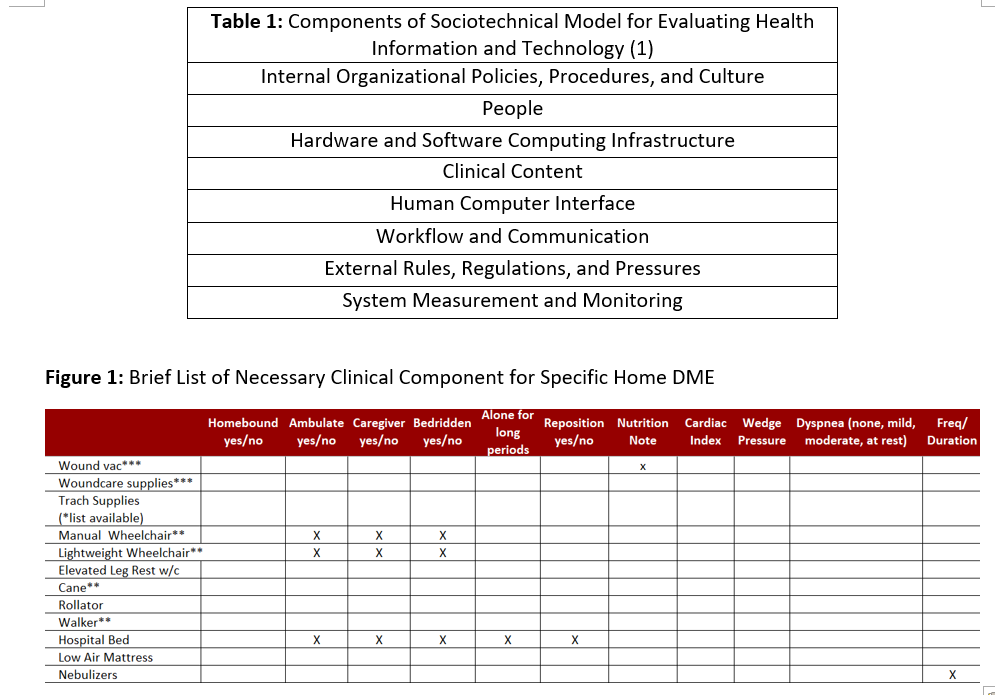
Background: In an increasingly digital world, there are still many manual and paper based workflows in healthcare. Paper scripts are an area that is prevalent and is the gold standard for certain prescribing behaviors. Paper scripts have numerous challenges, they can be lost, are difficult to track, and physically have to be delivered to the recipient. Home health and home durable medical equipment (DME) scripts are especially problematic. Often the doctor who ordered the equipment is unknown and it is next to impossible to figure out who is responsible in the event of an emergency or questions. Technology and the digitization of healthcare has offered an opportunity to improve paper based workflows. We used the sociotechnical model for evaluating health information technology as a framework for the development, deployment, and maintenance of a digital home health and home durable medical equipment (DME) electronic order (1).
Purpose: The aim of our project was to create a legally compliant and secure digital home health and home DME order and referral workflow that was trackable and clear for all healthcare providers.
Description: The sociotechnical model for evaluating health information and technology comprises of 8 parts (Table 1). We utilized all 8 parts to help build, deploy, and maintain our digital home health and home DME orders and process. The project’s first priority was to find an executive sponsor which may be unique to our organizational culture. The executive sponsor helped procure resources and support for the project. We assembled a multidisciplinary team of clinicians (residents and attendings), case managers, clinical informatics specialists, IT professionals, and executive leadership to help scope the project and agree on deliverables. We then evaluated legal and regulatory script for home health and home DME orders. Items such as NPI numbers, diagnosis codes, and compliance with security and privacy were addressed. We also confirmed with our Home Health and Home DME vendors that they would accepted a faxed electronic order. We next created a spreadsheet of all necessary clinical content for each unique Home Health and Home DME order (Figure 1). Now new hardware or software infrastructure was needed since we used our current electronic healthcare record, EPIC. The team iterated through numerous order designs to ensure each home health and DME order was (1) Comprehensive (2) Intuitive (3) Minimalistic. The availability of the electronic order was disseminated by electronic (emails) and in person (tipsheet, presentation) channels. Most effective were the case managers who championed the order by reminding all clinicians to order home health and home DME electronically. Case managers were supported by an icon that shows up on their patient list when a patient has a home health and/or home DME order. The orders are currently live and being evaluated monthly for the first three months, then in 3 months, then in 6 months, and then yearly. Each evaluation period will be looking to enhance the usability of the electronic order. Outcome and process metrics will be available shortly.
Conclusions: We successfully created an electronic order and referral process for home health and home DME orders. The trackable order has been accepted by all of our external vendors and has dramatically improved the workflow for all healthcare professionals. The result also showed significant time saving for both providers and case managers. This is a generalizable solution for other institutions looking to improve their discharge workflow.