Background: Patients admitted to our hospital with chest pain concerning for Acute Coronary Syndrome (ACS) have a length of stay exceeding the community average. We postulated that unnecessary stress test orders in some cases may be contributing to this increased length of stay. We hypothesized that implementation of a clinical decision support tool (CDST) would decrease the rate of cardiac stress test ordering and possibly decrease length of stay.
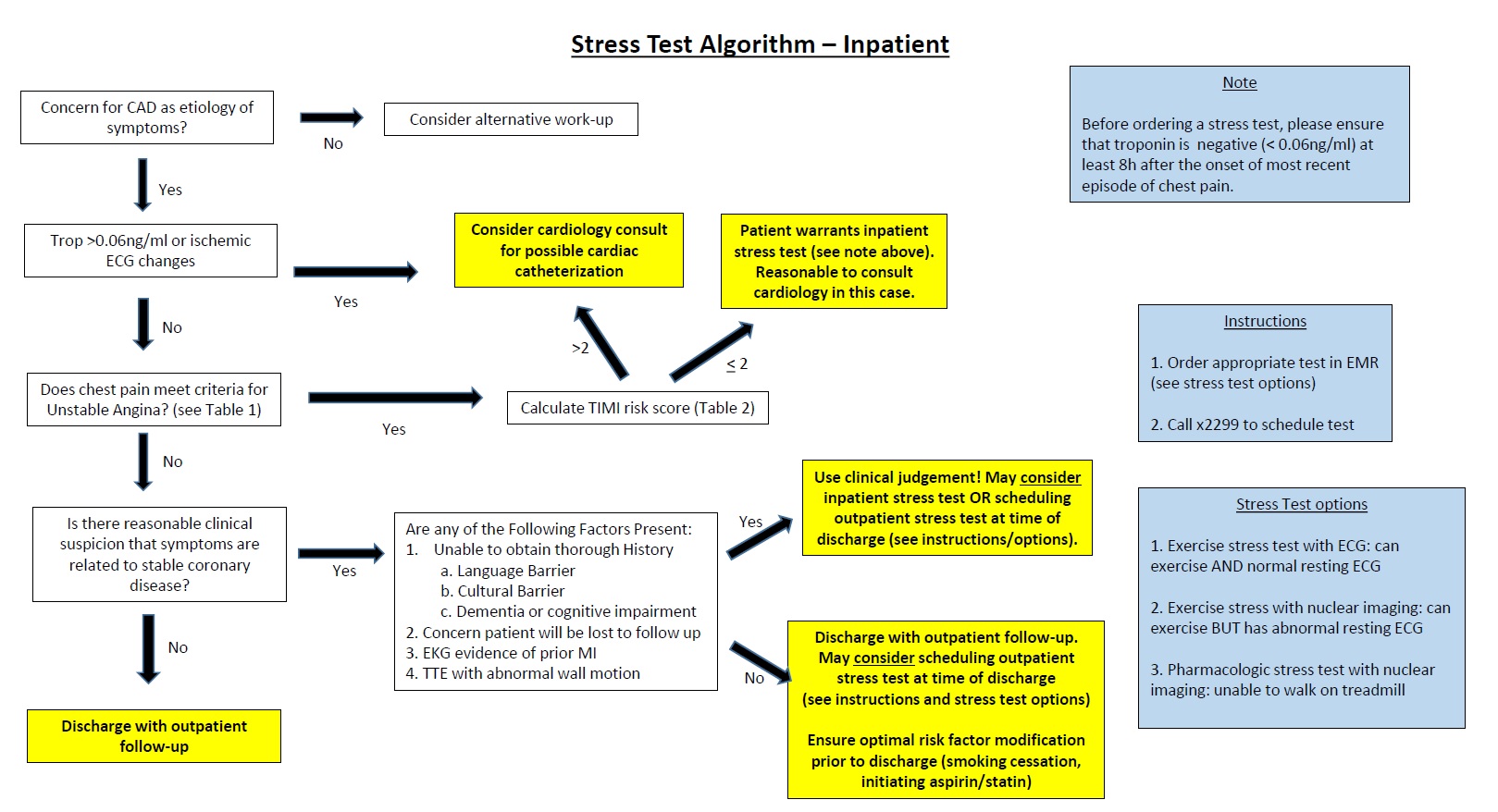
Methods: A pilot cardiac stress test CDST was developed at our institution and implemented on July 1, 2015. Based on reviews of initial data, local expertise from hospitalists and cardiologists, as well as feedback from discussions at SHM16, we created a revised CDST (Figure 1) that was distributed on July 1, 2016. We compared the cohort of patients admitted to the inpatient telemetry unit during the six months prior to implementation of the revised CDST (January through June 2016) with patients admitted during the one year after implementation (July 2016 through June 2017). The primary outcomes were the rate of stress test performed, the rate of positive stress test, and the average length of stay (ALOS).
Results: In the six months prior to the intervention 892 patients were admitted to telemetry, whereas in the year after the intervention 1,606 patients were admitted to telemetry. The rate of stress tests went from 19.8% (177/892) prior to the intervention to 15.2% (244/1,606) after the intervention (p = 0.0014). Baseline characteristics were the same among patients who had stress tests prior to the intervention compared to after the intervention, except for rate of “not on aspirin” (32% vs 42%, p=0.003) and rate of “not on statin” (32% vs 47%, p=0.001). The rate of positive stress test remained unchanged, going from 3.8% (34/892) prior to the intervention to 3.0% (48/1,606) after intervention (p = 0.18). The average length of stay went from 3.44 days prior to the intervention to 3.12 days after the intervention, however this difference was not statistically significant (p = 0.16).
Conclusions: The implementation of a CDST was associated with a significant decrease in the rate of inpatient stress tests performed at our hospital. The length of stay among patients on the telemetry unit also down-trended, though this was not statistically significant. While we performed fewer inpatient stress tests, the rate of positive stress test was unchanged, suggesting that the CDST decreased unnecessary testing without decreasing the rate of detection of coronary disease . Increasing provider use of the CDST has potential to further decrease unnecessary testing and further reduce ALOS, and may be achieved through embedding of the CDST into the electronic ordering system.