Background: Background: Advanced Practice Providers (APPs) are being increasingly utilized in hospital medicine groups. However, there is significant variation in how APPs are trained and utilized, resulting in high turnover rates, decreased provider satisfaction, and resistance to adopting a physician-APP practice model. Much of the literature around APP utilization is comparative in nature, describing APP performance and outcomes in comparison to that of physician counterparts. In contrast, there is minimal to no research focusing on the collaborative relationship between physicians and APPs. It is our belief that when utilized correctly, APPs can contribute to improved patient care, demonstrate a clear return on investment, and result in improved provider satisfaction. Currently, there are no defined ‘Best Practices’ around how to train, utilize, and sustain APP programs within medical groups.
Purpose: Purpose: Our aim is to identify and describe best practices in APP implementation, utilization and advancement within multidisciplinary medical groups. We hope to achieve this through the creation of a unifying platform to guide qualitative and quantitative research around factors which contribute to the successes and/or failures in APP utilization.
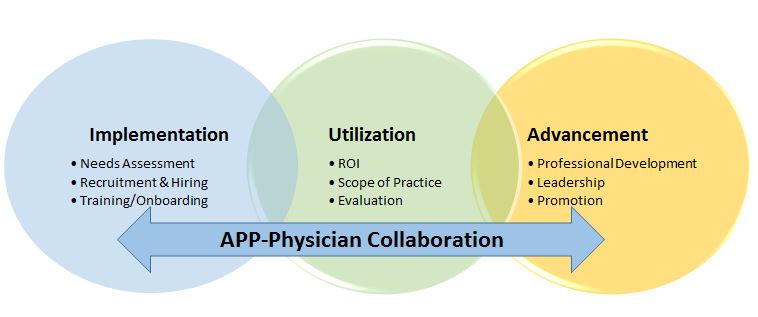
Description: Description: We have created a conceptual model to describe APP-Physician Best Practices. We first reviewed current literature around reasons for incorporating APPs onto medical teams, as well as intended outcomes for APPs. We found that APPs were largely incorporated with 3 main goals: improve patient care, demonstrate a clear return on investment, and improve provider morale. We then examined common barriers to achieving these goals, which included lack of standardization in training, lack of role clarity, and lack of opportunity for professional advancement. We combined these concepts into a framework for APP-Physician Best Practices. Our framework consists of 3 large domains: Implementation, Utilization and Advancement. Each domain has additional sub-categories. The implementation domain consists of: needs assessment, hiring processes, and training/onboarding. Utilization consists of ROI, scope of practice and evaluation, and advancement consists of professional development, leadership and promotion. Across all domains is a continuum of Physician-APP collaboration, which we believe is inherently necessary for APP success. We have started using this model in the University of Colorado Division of Hospital Medicine in various ways. For example, we recently completed a survey examining APP impact on physician burnout, are improving our onboarding program, and have begun work to create quality/productivity dashboards for APPs. We ultimately to develop APP-physician best practices for each large domain as well as each sub-category, which we intend to disseminate nationally.
Conclusions: Conclusions: Our conceptual model acts as a necessary guide to define, describe, and disseminate APP-Physician Best Practices. Defining APP-Physician Best Practices will be imperative to the continued growth and success of the APP profession.