Background: Most patients hospitalized with community-acquired pneumonia (CAP) can be safely treated with 5-days of antibiotic therapy. However, many are not. We aimed to determine whether a hospitalist-focused collaborative could reduce excessive antibiotic use in patients hospitalized with CAP through a combination of collaboration with antibiotic stewardship, data feedback, pay-for-performance, and sharing best practices.
Methods: From 4/2017-10/2018, trained abstractors in the Michigan Hospital Medicine Safety Consortium (HMS) collected data (medical record, phone calls 30-days after discharge) on a sample of adult, non-intensive care, patients hospitalized with CAP at 43 hospitals in Michigan. We used a guideline-based algorithm to determine appropriate antibiotic duration based on patient characteristics (e.g., clinical stability). The following were provided to all hospitals a) quarterly reports on rates of appropriate 5-day treatment (2016—current), b) best practices for reducing excess duration (2017—current) including a toolkit and webinar (3/2018), and c) pay-for-performance based on 5-day CAP metric (2018—current). Generalized linear mixed models, with hospital specific random intercepts, were used to evaluate change over time in a) proportion of patients with CAP eligible for 5-day treatment who received 5 ± 1 days and, after adjusting for patient characteristics, b) patient outcomes 30-days post-discharge.
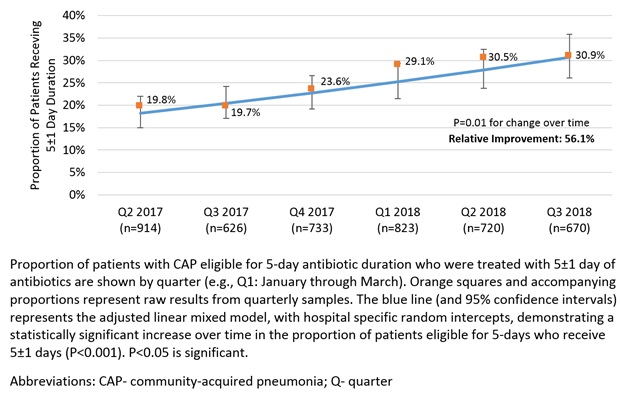
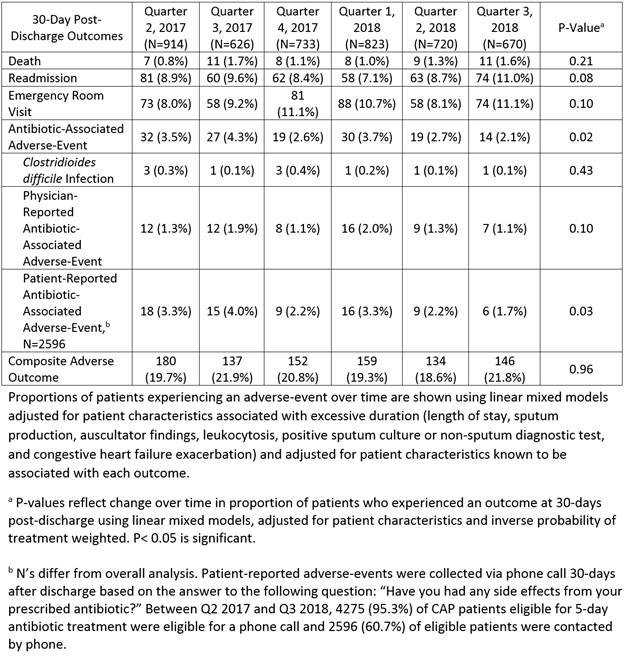
Results: Of 6,229 patients hospitalized with CAP, 4,769 (76.6%) were eligible for 5-days of antibiotic treatment; 283 (5.9%) did not have duration documented and were excluded. The majority of patients had severe pneumonia (50.3% with class IV/V pneumonia severity index) and were admitted by hospitalists (57.6%). Between 4/2017 and 10/2018, the proportion of patients eligible for 5-day antibiotic treatment who received 5 ± 1 days increased from 19.8% (181/914) to 30.9% (207/670; P=0.01), a relative improvement of 56.1% (Figure 1). During this same time period, there were no changes in 30-day post-discharge death, readmission, emergency room visit, Clostridioides (formerly known as Clostridium) difficile infection, or provider-documented antibiotic-associated adverse-events (Table 1). However, there was a statistically significant decrease (3.3% to 1.7%, P=0.03 for change over time; relative reduction: 48.5%) in patient-reported antibiotic-associated adverse-events.
Conclusions: A hospitalist-focused collaborative can safely reduce excess antibiotic duration and antibiotic-associated adverse-events in hospitalized patients with CAP.