Background: Timeliness in transitional care improves clinical outcomes by delivering medical care at the most vulnerable post-hospitalization time. Primary care access to in-network and out-of-network patients’ post-hospitalization has been a challenge, especially to sicker patients with high risk of readmissions. Our institution Post-Discharge Clinic bridges this need by developing processes that will improve timely transitional access according to the risk of readmission.
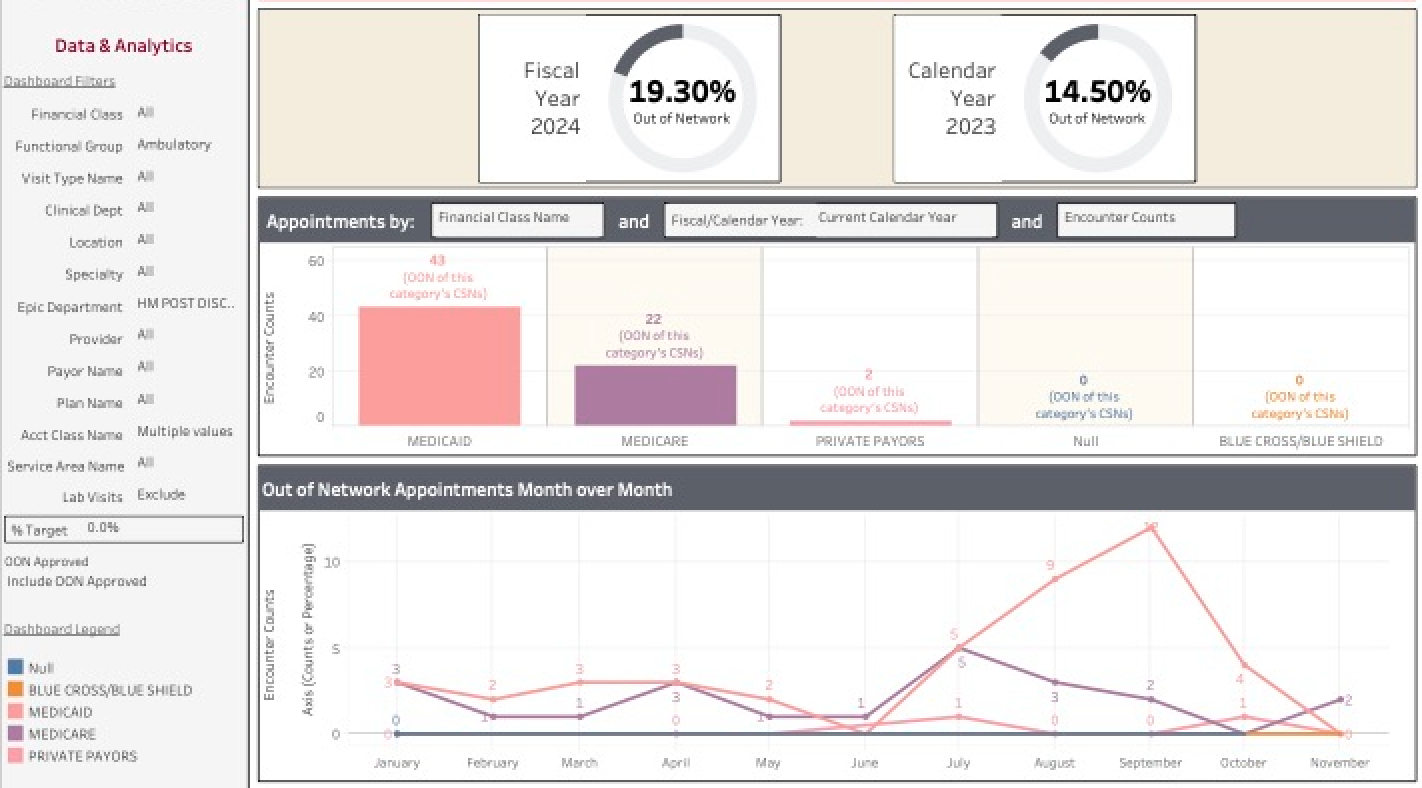
Purpose: To develop a seamless scheduling process for internal stakeholders and provide transitional care access to in-network (INN) and out-of-network (OON) patients within 7- and 14-days post-hospitalization according to the risk of readmission.
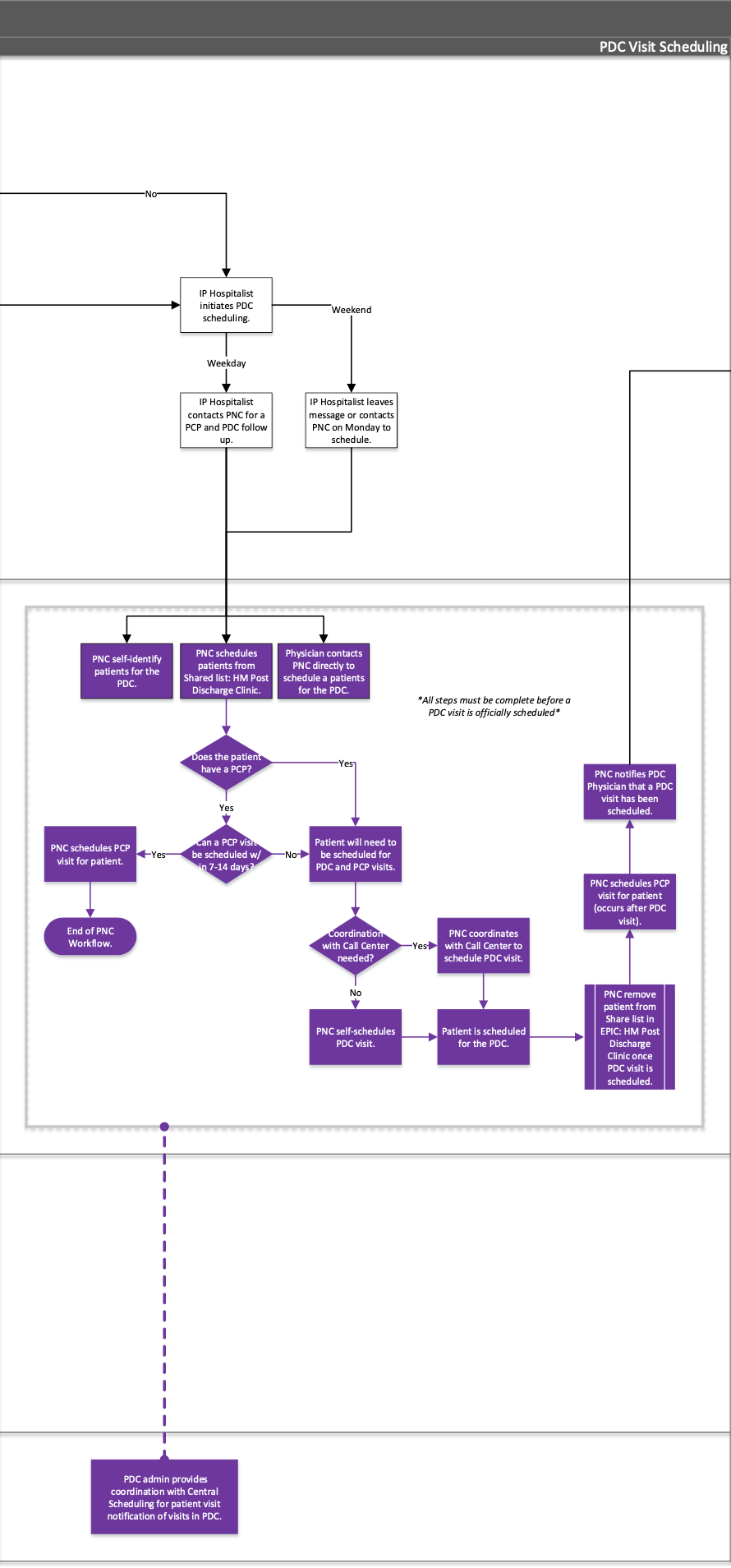
Description: When patients are in the hospital, it is difficult to schedule patients’ appointments without knowing outpatient appointment availability. Patient Navigator Coordinators (PNCs) do not have access to a scheduling view of available appointments as is present in outpatient settings and must rely on central scheduling for appointments without input from the patients. The Post-Discharge Clinic (PDC) developed processes that provide an easy access to PDC providers’ clinic schedule, allowing the PNCs to have overall view of openings in the schedule and offer available appointments to patients as needed. Furthermore, the decision of when patients should be seen is critical to scheduling. The PDC in partnership with the Office of Clinical Transformation developed processes to risk-stratify scheduling for patients with high risk of readmissions to be seen within 7 days post-hospitalization vs patients with other risk within 14 days post-hospitalization. PDC provides the flexibility to open PDC clinic sessions if the demand exceeds the capacity within 14 days post-hospitalization. PDC provides face-to face sessions for sicker patients or patients who prefer to being seen in-person, and virtual sessions for sicker patients who are unable to come to appointments or patients who prefer to being seen virtually. We received financial support from the institution to provide cost-effective transitional care for the out-of-network population that meet criteria for increased close post-discharge surveillance, to decrease length of hospitalization or risk of readmission.
Conclusions: Timely access is critical to the sicker population we serve. An innovated approach of scheduling, coordination with the leadership of Office of Clinical Transformation and Finance allows us to care for INN and OON patients. Our innovative processes have produced an increased capacity for in-network and out-of-network patients and serve as major contributors to provide decreased rate of readmission and return visits of our most vulnerable populations.