Background: Lack of mobility amongst inpatients is prevalent and deleterious. Hospitalized patients have been shown to spend an average of 83% of their stay in bed, leading to complications including loss of independence in activities of daily living, lower rates of discharge to home, worsening length of stay, and increased mortality. Programs to increase inpatient mobility have involved assessing mobility throughout the hospital stay through a standardized measure, door signs to communicate mobility status, development of exercises aimed at mobility, and designation of specific mobility roles amongst nurses or patient care technicians. Unfortunately, difficulty in achieving optimal staffing has limited incorporation of pro-mobility measures in many hospitals.
Purpose: We are instituting a culture of mobility at the Medical University of South Carolina. We standardized interdisciplinary assessment and communication of mobility using the Activity Measure for Post-Acute Care (AM-PAC) with all inpatients and introduced door signs and mobility games for patient engagement. Given limited resources, we aim to identify patients that would be most likely to benefit from a low effort, high impact intervention. In the next phase of our project, we plan to initiate an interprofessional mobility curriculum for university students that includes direct patient mobilization.
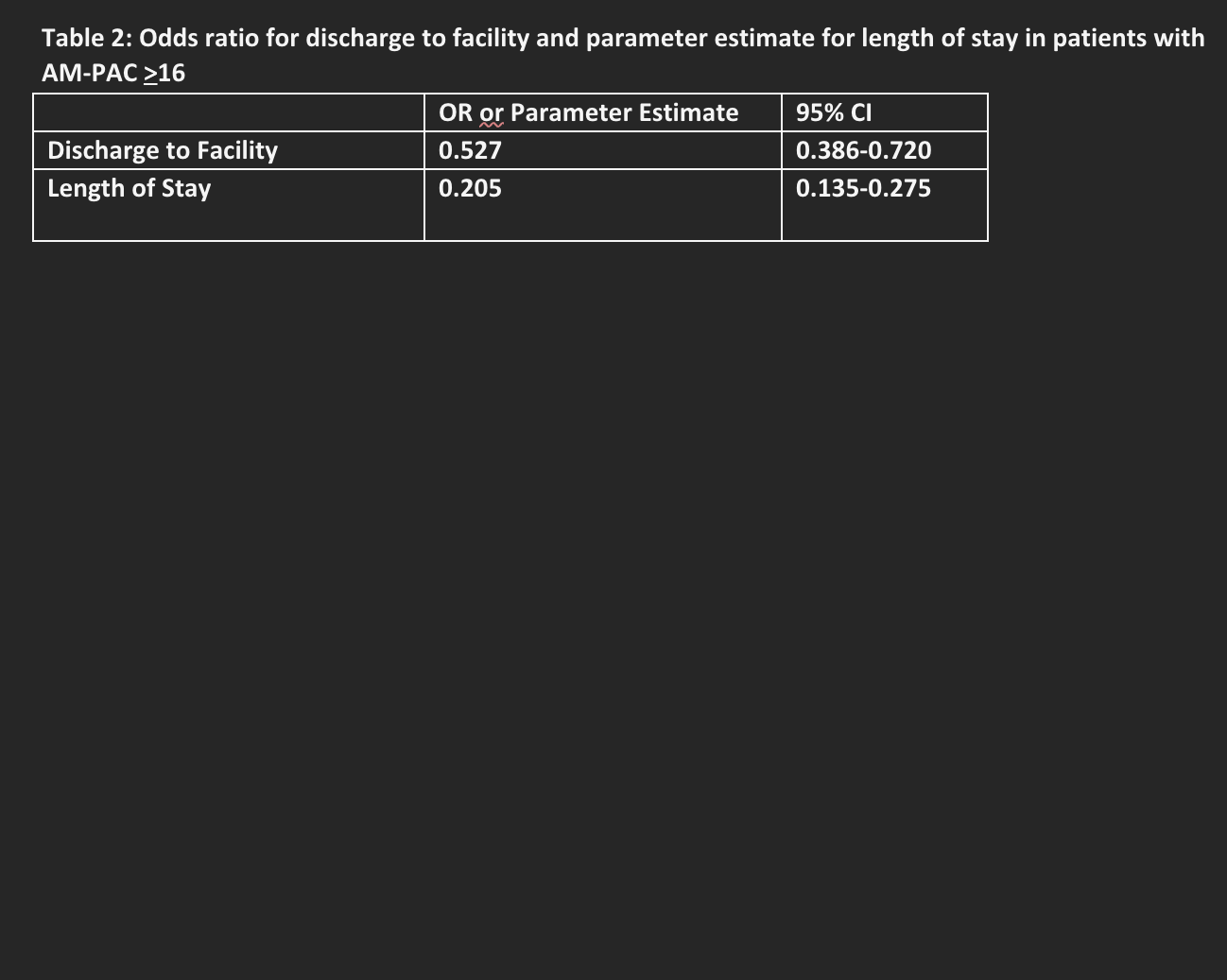
Description: To begin, we identified patients with an AM-PAC score of 16 or above which indicates a patient able to ambulate. Taking this subset of patients (AMPAC ≥16), we assessed whether ambulation during admission would affect discharge disposition (home vs facility) or length of stay. Our next phase will be to initiate our educational intervention, consisting of an interprofessional course to emphasize the importance of mobility, teach safe mobilization techniques, and provide direct contact hours for students to directly mobilize patients.
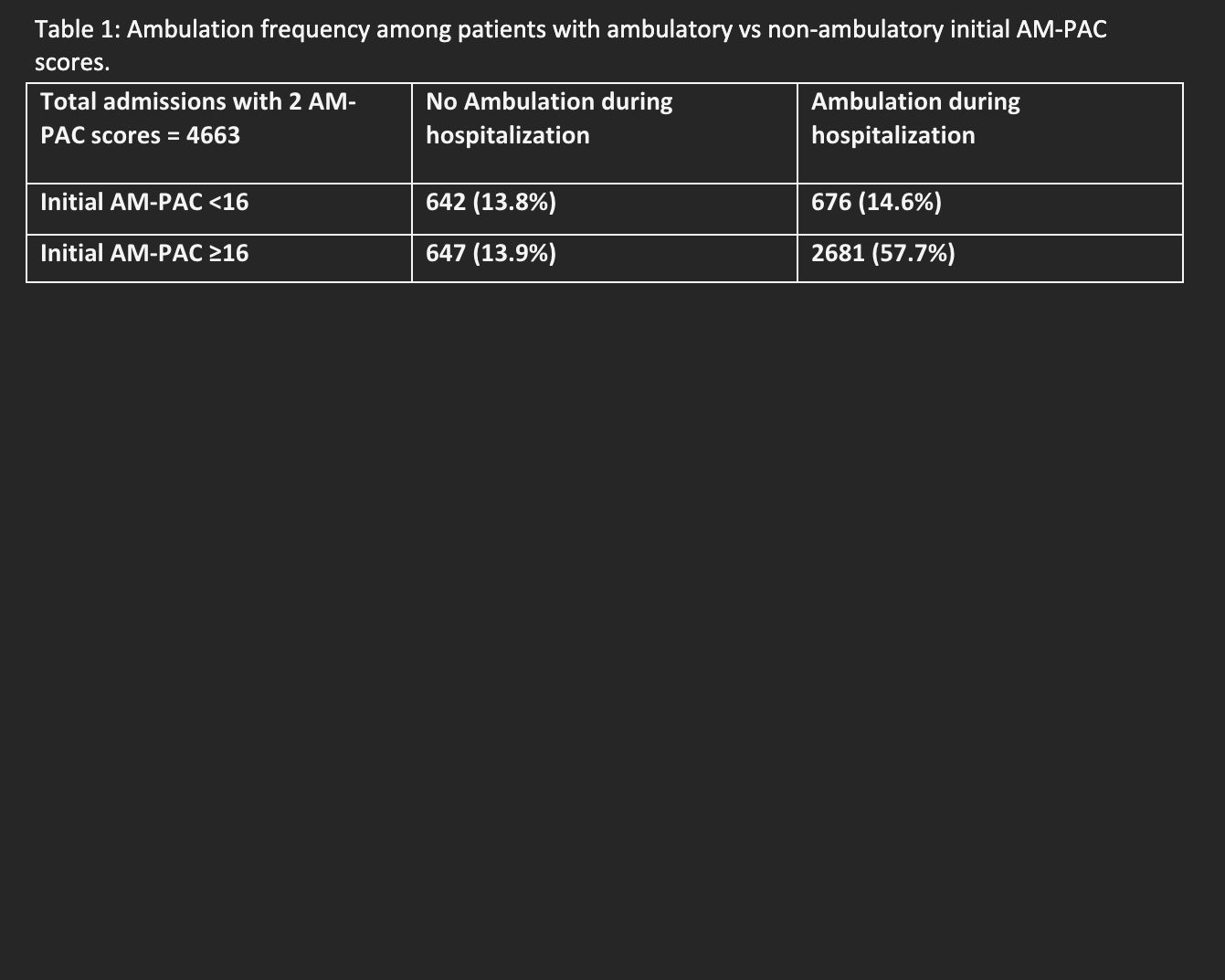
Conclusions: Discharges from July-September 2023 showed significant uptake of new documentation goals: 61.4% of patients (4663/7610) had at least 2 AM-PAC scores recorded during their hospitalization. Nurses also documented ambulation during admission in binary terms (yes/no). Among inpatients initially appropriate for ambulation (first AM-PAC ≥16), 80.6% (2681/3328) did ambulate during their hospitalization (Table 1). Controlling for demographics, Charlson Comorbidity Index (CCI) and primary diagnosis group, patients who ambulated had 47% lower odds (0.527, 95% CI 0.386-0.720) of discharge to facility (Table 2). Additionally, contrary to our hypothesis, ambulation was correlated with an increased length of stay by 0.2 days (95% CI 0.13-0.27), with the same control variables. Based on our findings, we will further assess patients with AM-PAC > 16 and focus our educational intervention on patients who will likely benefit the most.