Case Presentation: A 42-year-old man was diagnosed with AIDS after presenting to his PCP for subacute subjective fevers, unintended weight loss, headache, and generalized malaise. He was referred to infectious diseases and was started on Biktarvy for ART as well as Bactrim and Zithromax for prophylaxis for a CD4 count of 18 cells/mm3 and HIV viral load of 57,300 copies/mL. One week later, the patient experienced the sudden onset of painless binocular decreased visual acuity and bilateral lower extremity weakness, leading to a car accident. Given non-resolution of his symptoms and evolving nausea and vomiting over the ensuing hours, the patient presented to the ED. He was initially afebrile and hemodynamically stable. Physical examination was notable for a fully conversant and pleasant gentleman able to move all four extremities with full upper extremity strength and symmetrically reduced (4+/5) lower extremity strength. Furthermore, examination disclosed a left-sided cranial nerve VI palsy, and the absence of both papilledema and nuchal rigidity. Labs showed a normal white blood cell count and a serum sodium of 126 mEq/L (previously normal). Both non-contrast CT of the head and CT angiography of the head and neck were negative. MRI, however, revealed findings suspicious for left anterior cerebral artery territory ischemia. During his first day of hospitalization, he experienced multiple seizures. He was moved to the neurological intensive care unit, where he underwent a lumbar puncture notable for normal protein (36 mg/dL), decreased glucose (21 mg/dL), elevated opening pressure (52 cm H2O), and Gram stain and culture revealing Cryptococcus neoformans. Liposomal amphotericin B and flucytosine were started to treat cryptococcal meningitis, and ART was discontinued. Serial lumbar punctures were performed, each of which was notable for sustained elevated opening pressures. The next day, the patient herniated and was declared brain dead.
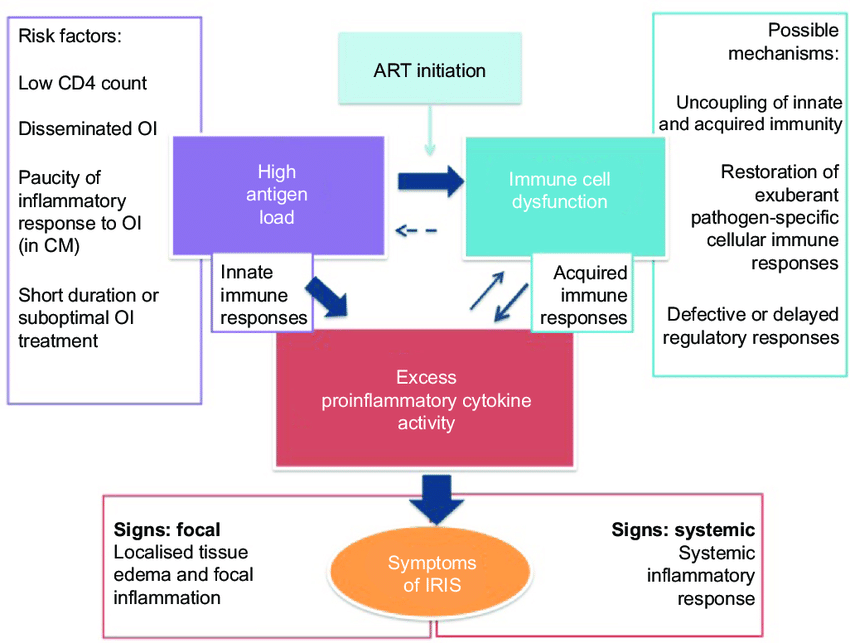
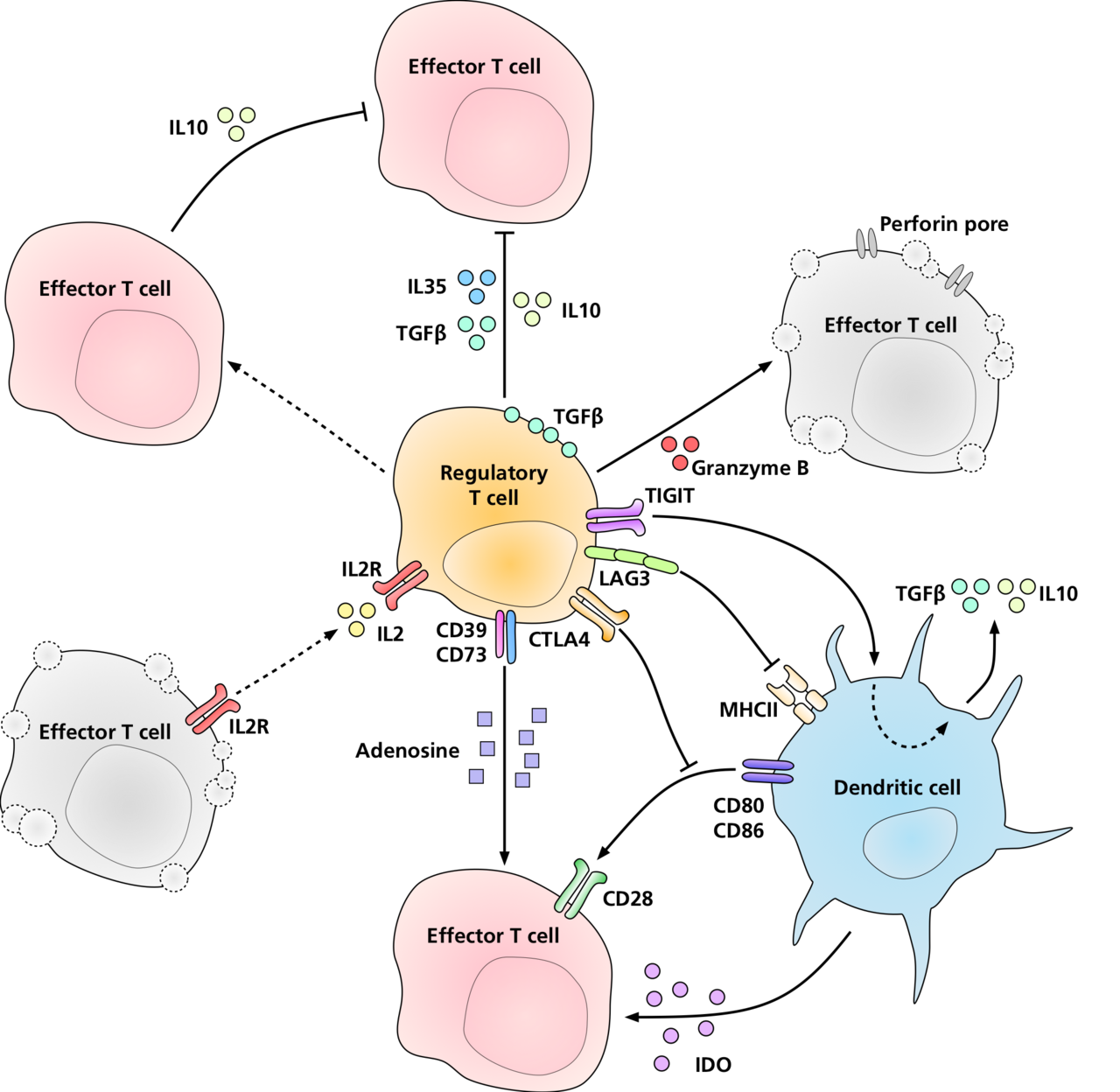
Discussion: The immune reconstitution inflammatory syndrome (IRIS) is a dysregulated immune response in HIV/AIDS patients who have recently started antiretroviral therapy (ART). Specifically, an imbalance between pro-inflammatory and regulatory CD4+ populations are thought to be central in the pathogenesis of IRIS. This case offers a fascinating, albeit tragic, opportunity for insight into reviewing the pathophysiology of IRIS, its two phenotypes, a review of risk factors to stratify which patients are at the highest risk for developing IRIS, and management.
Conclusions: Ultimately, the pathophysiology of IRIS is rooted in a dysregulated reconstitution of CD4+ T-Cells – namely, an imbalance between regulatory lines (i.e.: Tregs) and the pro-inflammatory lines (Th17) leads to an overall imbalanced and exaggerated response to antigens. There are two clinical phenotypes by which IRIS manifests – the unmasking phenotype, in which ART initiation unmasks a previously-occult opportunistic infection, and the paradoxical phenotype, in which ART initiation causes paradoxical worsening of an already-existing opportunistic infection. In general, at-risk patients include those with lower CD4 counts at the time of ART initiation (highlighting the critical role of early HIV diagnosis in the prevention of IRIS), ART-naïve patients, patients with faster decreases in HIV viral load, and mycobacterial or cryptococcal species. Management considerations include decisions as to whether to continue or hold ART and which anti-inflammatory strategy is most effective.