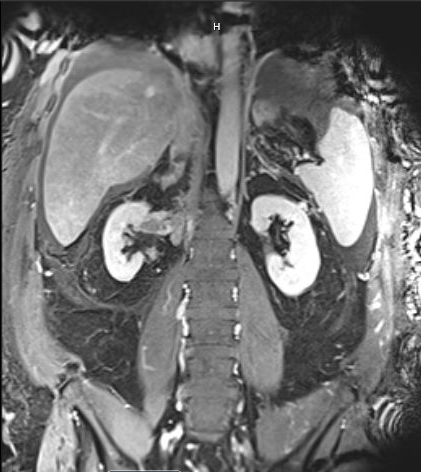
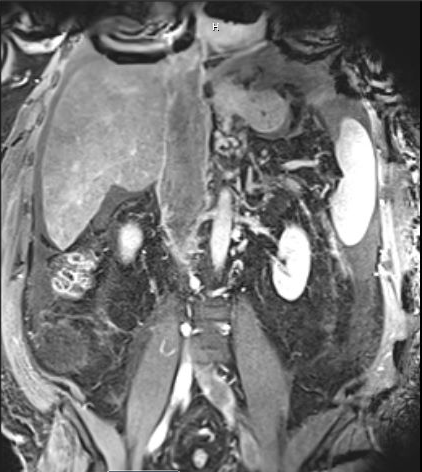
Case Presentation: Introduction: Renal cell carcinoma (RCC) is classically associated with the triad of abdominal pain, hematuria, and a palpable mass, but its variability in clinical presentation has earned it the label of “internist’s tumor” (1,2). Liver dysfunction has been observed as a result of metastatic disease and a non-metastatic paraneoplastic syndrome called Stauffer’s syndrome (3,4). Additionally, RCC can extend through the renal vein into the inferior vena cava (IVC), extend intra-luminally with tumor thrombus formation occurring in 5-15% of cases, and extension to the right cardiac chambers in 1% of cases (5). Here we present a case of cryptogenic cirrhosis as the initial clinical presentation of newly diagnosed RCC with a large IVC tumor thrombus burden extending to the right atrium. Case: A 58M with a history of HTN, DM2 and IgA nephropathy of the left kidney admitted with right-sided abdominal pain, fatigue, and left-sided lower extremity edema of six weeks’ duration. He was evaluated at another facility one week prior to presentation and was diagnosed with cryptogenic cirrhosis. Upon admission to our facility, exam was notable for 4+ pitting LLE edema and 2+ pitting RLE edema, a slightly distended abdomen without a fluid wave, RUQ tenderness to palpation. Labs were notable for creatinine 2.47 (unknown baseline), mildly elevated AST, ALT, total bilirubin, and lactate, and elevated alkaline phosphatase and LDH. Platelets, INR, and albumin were within normal limits.Initial imaging showed acute DVT in the LLE extending into the IVC. He was started on systemic anticoagulation with plan for thrombolysis. Subsequent imaging revealed infiltrative right upper pole/interpolar renal mass with associated large volume tumor thrombus (involving right renal vein, IVC, left renal vein, left gonadal vein, T12/L1 right lumbar vein, right hepatic vein, and right atrium), evidence of IVC wall invasion, chronic pulmonary embolism, and severe congestive hepatopathy from venous outflow obstruction with ascites and varices. Transvenous biopsies of the IVC thrombus revealed RCC, the subtype of which could not be determined. Additional imaging showed no evidence of metastatic disease.Radical right nephrectomy and IVC thrombectomy was planned; however, the day prior to surgery, patient was found to have an acute subdural hematoma. Patient’s neurological status declined significantly and patient died in inpatient hospice. No autopsy was done.
Discussion: This case highlights a rare presentation of veno-invasive RCC extending to the right atrium, resulting in cirrhosis. Although hepatic dysfunction is seen in 10-15% of patients with RCC (4), frank cirrhosis has, to our knowledge, not previously been reported in the literature as the presenting sign of RCC. Additionally, this patient originally presented with a diagnosis of cryptogenic cirrhosis that could have ostensibly explained his bilateral lower extremity edema and abdominal pain. However, further evaluation revealed the underlying unifying diagnosis, highlighting the need for adopting a critical view of previous diagnoses at the time of admission.
Conclusions: RCC has a clinically variable presentation that requires a high clinical suspicion to recognize. Our patient had a very rare initial presentation of cirrhosis caused by veno-occlusive disease from an extensive IVC tumor thrombus burden that extended all the way to the right atrium.