Background: Among survivors of ischemic stroke (IS), the cumulative long-term burden of readmissions, determinants of readmission, and clinical consequence of hospital readmission remain poorly understood. we aimed to investigate 1) the cumulative incidence of readmission; 2) at-risk patient for readmission, 3) the effect of readmission on subsequent mortality; and 4) whether the days spent in hospital during the follow-up is predictive of subsequent mortality.
Methods: Adults who survived hospitalization for first AIS from 2003 through 2018 were followed for readmissions, days and percentage of time spent hospitalized and subsequent long-term mortality. Poisson regression models were generated to determine independent predictors of cumulative repeat hospitalizations. Separate Poisson regression models were developed to estimate incident rate ratio (IRR) for all-cause, cardiovascular (CV), and non-cardiovascular (non-CV) hospitalizations.Multiple time-dependent Cox proportional regression models were constructed to estimate hazard ratio (HR) for each category of readmission (all-cause, CV and non-CV) separately for incident death from any cause and stroke, CV, or non-CV condition.
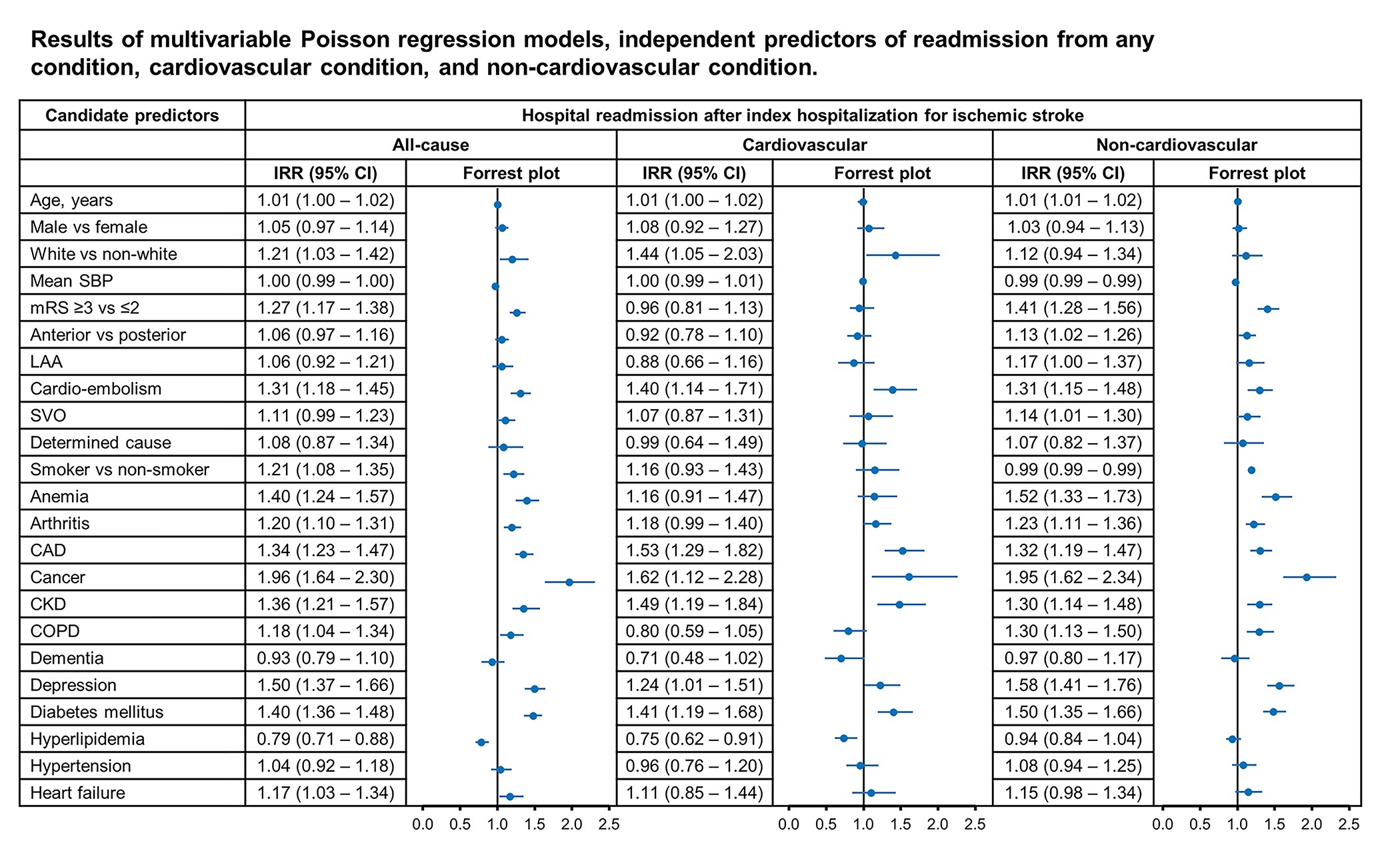
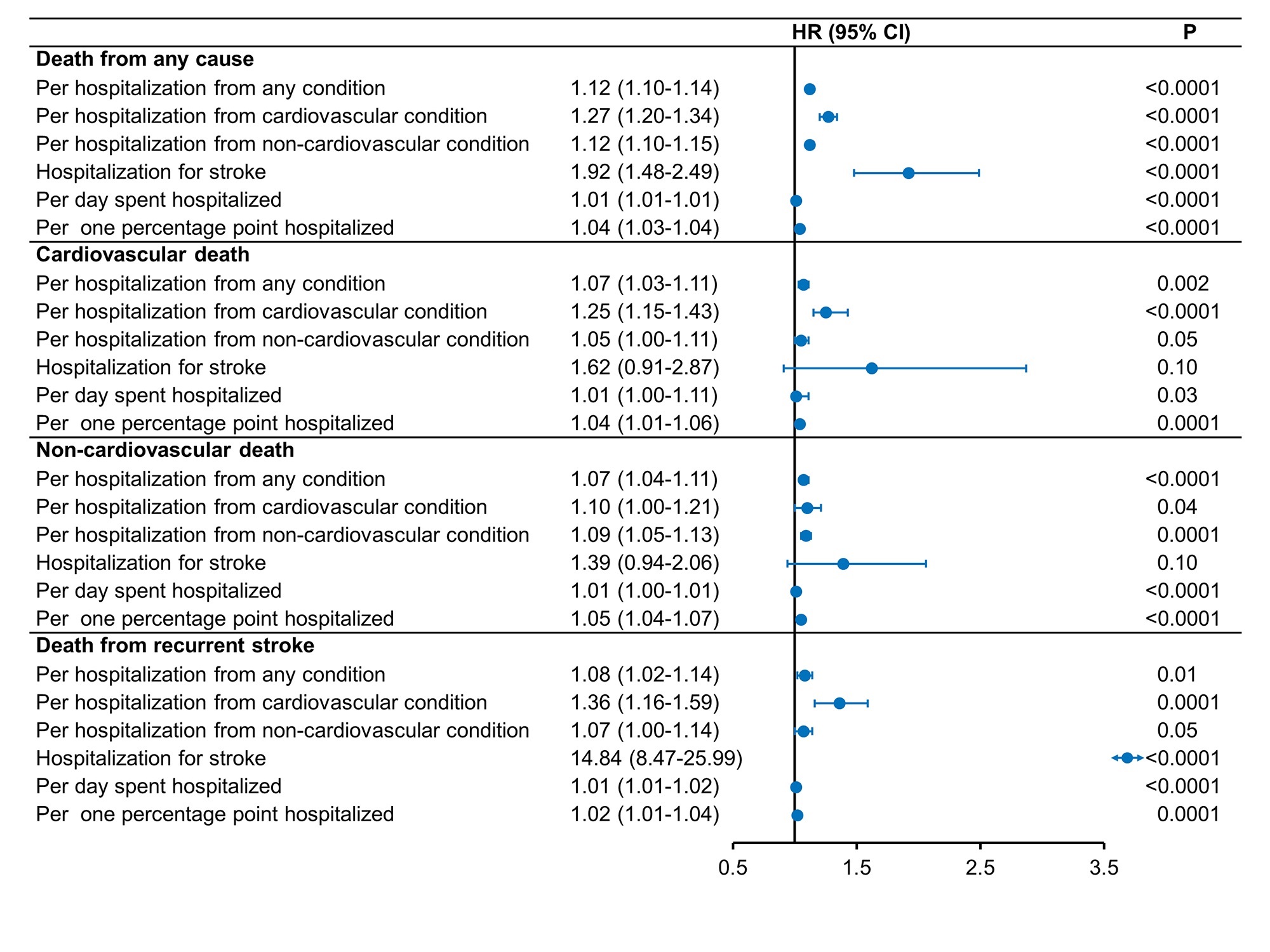
Results: Of 907 patients discharged alive after IS, 548 (60%) died, 669 (74%) had 2,645 all-cause readmission (cardiovascular 715 [27%], non-cardiovascular 1,944 [63%]) with 12,089 days hospitalized during 4,535 person-years of follow-up. After adjustment, increasing age (Incidence rate ratio [IRR] 1.01, 95% confidence interval [CI] 1.00 – 1.02), white ethnicity (IRR 1.21, 95% CI 1.03-1.42) dependency at discharge (IRR 1.27, 95% CI 1.17-1.38), cardio-embolism (IRR 1.35, 95% CI 1.18 – 1.45), current smoking (IRR 1.21, 95% CI 1.08 – 1.35), anemia (IRR 1.40, 95% CI 1.24 – 1.57), arthritis (IRR 1.20, 95% CI 1.10 – 1.31), coronary artery disease (IRR 1.34, 95% CI 1.23 – 1.47), cancer (IRR 1.96, 95% CI 1.64 – 2.30), chronic kidney disease (IRR 1.36, 95% CI 1.21 – 1.57), chronic obstructive pulmonary disease (IRR 1.18, 95% CI 1.04 – 1.34), depression (IRR 1.50, 95% CI 1.37 – 1.66), diabetes mellitus (IRR 1.48, 95% CI 1.36 – 1.48), and heart failure (IRR 1.17, 95% CI 1.03 – 1.34) were all associated with higher risk while hyperlipidemia (IRR 0.79, 95% CI 0.71 – 0.88) was associated with a lower risk of all-cause readmission. All-cause mortality was significantly increased after each hospitalization (hazard ration [HR] 1.12, 95% CI 1.106 -1.14), and each day (HR 1.01, 95% CI 1.01 – 1.01) and each 1% of follow-up time spent hospitalized (HR 1.04, 95% CI 1.03 – 1.04).
Conclusions: The findings of the present study characterized the groups of AIS survivors at high risk for hospital readmission and estimated the effect of each readmission and days hospitalized on subsequent mortality after initial AIS hospitalization. Our results reinforces the importance of several patient-level characteristics including comorbid conditions and assist clinician and policy makers in developing strategies aimed at preventing readmissions and thereby reducing the risk of death following IS.