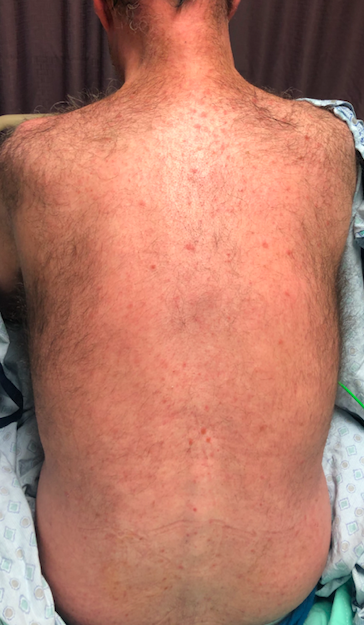
Case Presentation: A 44-year man with history notable for illicit drug use (amphetamine, cocaine), poorly controlled HIV (CD4 count 387, HIV quantitative PCR with a viral load of 188,000) and anaphylaxis with penicillin use presented with a 1-day history of sore throat along with a 1-month history of a warm, diffuse, symmetric, non-pruritic, non-vesicular, maculopapular rash. His rash first developed on his trunk and gradually spread across his entire body involving the genital area and extremities, including his bilateral palms and soles. Mucosal surfaces were spared. He was alert and oriented to person, place and date. He had an unremarkable neurological exam without neck stiffness, gait abnormalities, vision or hearing problems. Pupillary response to light and accommodation was intact bilaterally. He tested positive for syphilis with elevated serum RPR (1:64) and reactive FTA-ABS. His HIV was poorly controlled with low peripheral blood CD4 + T cell count and detectable plasma HIV RNA. Because of this, he underwent lumbar puncture despite his lack of neurological symptoms. His central spinal fluid (CSF) VDRL was reactive and a diagnosis of asymptomatic neurosyphilis was made. He underwent penicillin desensitization and was treated with intravenous penicillin with plans for a 14-day course.
Discussion: Neurosyphilis refers to infection of the central nervous system by Treponema pallidum, the spirochete causing syphilis. Traditionally, it was thought that neurosyphilis occurs only with later stages of syphilis, however, since the re-emergence of syphilis during the HIV epidemic it has become clear that neurosyphilis can co-occur with early stages of syphilis in both HIV infected and non-infected patients. Patients with poorly controlled HIV have a higher incidence of both asymptomatic and symptomatic neurosyphilis, highlighting the importance of considering this investigation at the time of syphilis diagnosis.
Conclusions: This case illustrates the significance of having a high clinical suspicion for neurosyphilis at the time of syphilis diagnosis and a low threshold for lumbar puncture and CSF analysis, especially in patients with poorly controlled HIV. While it is unknown whether diagnosing asymptomatic neurosyphilis changes outcomes in the era of antibiotics, treatment of neurosyphilis involves more intensive antibiotic therapy than syphilis without CNS involvement. In our patient’s case, the initial plan was to treat the patient for secondary syphilis with a single dose of intramuscular penicillin G benzathine, however, once he was diagnosed with neurosyphilis his treatment plan was changed to intravenous penicillin for 14 days. Failure to treat asymptomatic neurosyphilis appropriately may result in progression to symptomatic neurosyphilis with serious consequences such as impairment in vision and hearing, stroke, general paresis or tabes dorsalis.