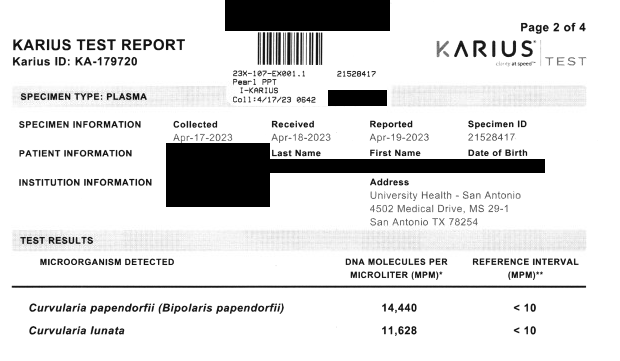
Case Presentation: A 67-year-old male presented to the Emergency Department with a chief complaint of bilateral vision loss. He had a complex medical history including atrial fibrillation, coronary artery bypass graft surgery, aortic stenosis with bioprosthetic valve replacement, and ascending aortic aneurysm graft and repair performed in 2022. He was admitted and on inpatient work-up was found to have bilateral panuveitis and retinal dysfunction. CT angiography of the abdomen and pelvis revealed splenic wedge infarcts that, with the patient’s initial presentation of sudden vision loss, could demonstrate thromboembolic disease. CT angiography of the chest also demonstrated a 2.8 x 1.5 cm hypodensity along the periphery of his ascending aortic graft that was concerning for infectious aortitis versus a thrombus. He was transferred to the Cardiac ICU for treatment of his possible ascending aortic clot. Cultures of the site were taken on hospital day 10. He was anticoagulated with warfarin. The patient’s Karius test resulted, revealing the growth of 14,440 MPM Curvularia papendorfii and 11,628 MPM Curvularia lunata.His hospital stay was complicated by severely altered mental status, and on imaging was found to have bilateral temporo-occipital parenchymal hemorrhages. He was transferred to the Neuro ICU for neurosurgery evaluation. After goals of care discussions with his healthcare team and medical power of attorney, his family opted to pursue comfort care measures. The patient was discharged home with hospice. The family had requested an autopsy of the aortic graft and was instructed to notify the healthcare team once applicable.
Discussion: Aortic graft infections are rare but are increasing in incidence in patients undergoing vascular procedures, such as aortic aneurysm and dissection. These infections are most commonly caused by Staphylococcus aureus and are associated with high mortality and reinfection rates1, 5. Curvularia species is a dematiaceous fungi (aka ‘black fungi’) typically found in tropical environmental sources such as soil and plant debris, but has clinical relevance as an opportunistic pathogen in corneal, cutaneous, and subcutaneous infections, with most cases occurring in immunocompetent patients 2,3. We present a unique case of a patient with an aortic graft infected by Curvularia Papendorfii.
Conclusions: On review of current literature, the majority of documented mycotic infections by Curvularia species and other dematiaceous fungi have been cutaneous, corneal, and sinus tract infections in immunocompetent patients. Disseminated mycoses occur in immunocompromised individuals, most commonly manifesting as cerebral infection, and more rarely as endocarditis. There have been very few case reports of dematiaceous endocarditis, with one case report of prosthetic valve endocarditis highlighting the successful treatment with combination antifungal therapies (prompt surgical intervention in combination with amphotericin B, voriconazole, ketoconazole, and terbinafine)4. However, there are no documented cases of Curvularia papendorfii infection of an aortic graft. Only two other case studies describe similar presentations of fungal endarteritis following ascending aortic grafting and aortic valve replacement attributed to Bipolaris species, a genus closely related to Curvularia species but morphologically dissimilar6, 7. This case highlights the presentation of a rare fungal infection by Curvularia papendorfii of an ascending aortic graft.