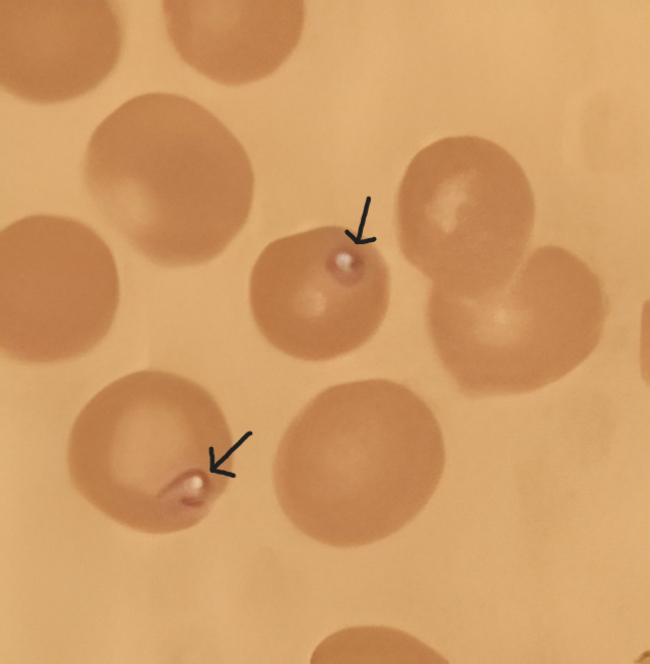
Case Presentation: A 46-year-old woman with a past medical history of breast cancer, on tamoxifen, presented to the hospital for two-day history of progressive and generalized rash with a fever. Two weeks prior, she took cephalexin for one week for cellulitis of her right lower leg. The patient did not report a recent travel history. The patient was febrile to a temperature of 100.6 F. Physical examination was remarkable for generalized erythematous maculopapular rash with diffuse non-blanching petechiae of the bilateral lower extremities. Initial laboratory investigations were remarkable for thrombocytopenia, reticulocytosis, raised LDH, D-dimer, and CRP, and decreased haptoglobin. WBC counts, renal function, liver function tests, coagulation profile, ANA, cryoglobulin, urine studies, and peripheral smear were unremarkable. Blood cultures, viral respiratory panel, serologies for EBV, CMV, hepatitis virus, HIV, HSV DNA, Lumbar Puncture, and echocardiography were negative. Over subsequent days, the patient developed worsening headache, fevers, progressive thrombocytopenia, worsening LFTs, and decreasing hemoglobin. She was started on IV Doxycycline to cover the common tick-borne illnesses. CT scan abdomen and pelvis was remarkable for hepatosplenomegaly. On hospital day 10, azithromycin and atovaquone were started for confirmed babesiosis, which was diagnosed through the Karius test, with positive babesia specific antibodies and 1 % parasite burden on peripheral smear. Doxycycline was continued due to positive Lyme Serology. Raised ferritin and triglycerides led to a suspicion for HLH. Bone marrow biopsy revealed normocellular marrow with maturing trilineage hematopoiesis and numerous trophozoites, consistent with babesiosis and few histiocytes showing hemophagocytosis. The patient improved clinically and was discharged on Day 21 with oral atovaquone and azithromycin. By Day 28, her symptoms had fully resolved, and her blood test results showed improvement during her clinic visit.
Discussion: Babesiosis is a tick-borne disease, transmitted by Ixodes scapularis and caused by the protozoan Babesia. The recent rise in the incidence of Babesiosis is a national concern in the United States. Babesiosis is mostly a self-limited disease, however rare, more severe complications have been reported in immunocompromised patients. Our case describes how Babesiosis can be a diagnostic challenge without a typical exposure history. Our patient, who is young and immunocompetent, developed HLH from a co-infection of babesia and Lyme disease, which goes against the 9 cases reporting HLH in immunocompromised patients.
Conclusions: Our case highlights the importance of realizing anchoring bias. While a rash linked to antibiotic use may indicate a drug reaction, clinicians should also consider tick-borne infections as a potential cause of febrile illness with rash, particularly during the summer.