Background: Drug overdose deaths are increasing throughout the country. Increasing naloxone availability is a cost-effective way to prevent opioid-related deaths. High-risk patients admitted in the hospital may benefit from a take-home naloxone prescription. This study aims to assess naloxone prescribing practices upon hospital discharge.
Methods: An anonymous survey was distributed to attendings, residents, and advanced practice providers (APPs) in our institution’s Division of Hospital Medicine and residency programs in Internal Medicine/Med-Peds. Using a 5 point Likert scale, providers were questioned on their level of agreement in prescribing naloxone to specific patients and on barriers in prescribing naloxone at discharge. Statistical analysis was performed using Kruskal-Wallis, chi-square, and Fisher’s exact tests to assess differences between providers.
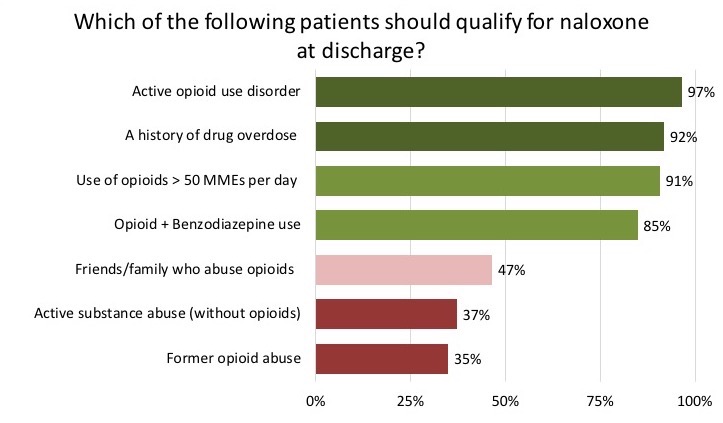
Results: The survey response rate was 52% (92/178), with 39 attendings, 43 residents, and 10 APPs. See Figure 1 and Figure 2 for overall response results of naloxone prescribing practices in high-risk populations and barriers in prescribing naloxone at discharge, respectively. Greater than 90% of respondents agreed that naloxone should be prescribed for patients with an active opioid use disorder, history of overdose, and use of greater than 50 morphine milligram equivalents per day. More residents compared to attendings reported that patients with friends/family with a substance use disorder should be prescribed naloxone (61% vs 37%, p=0.024).
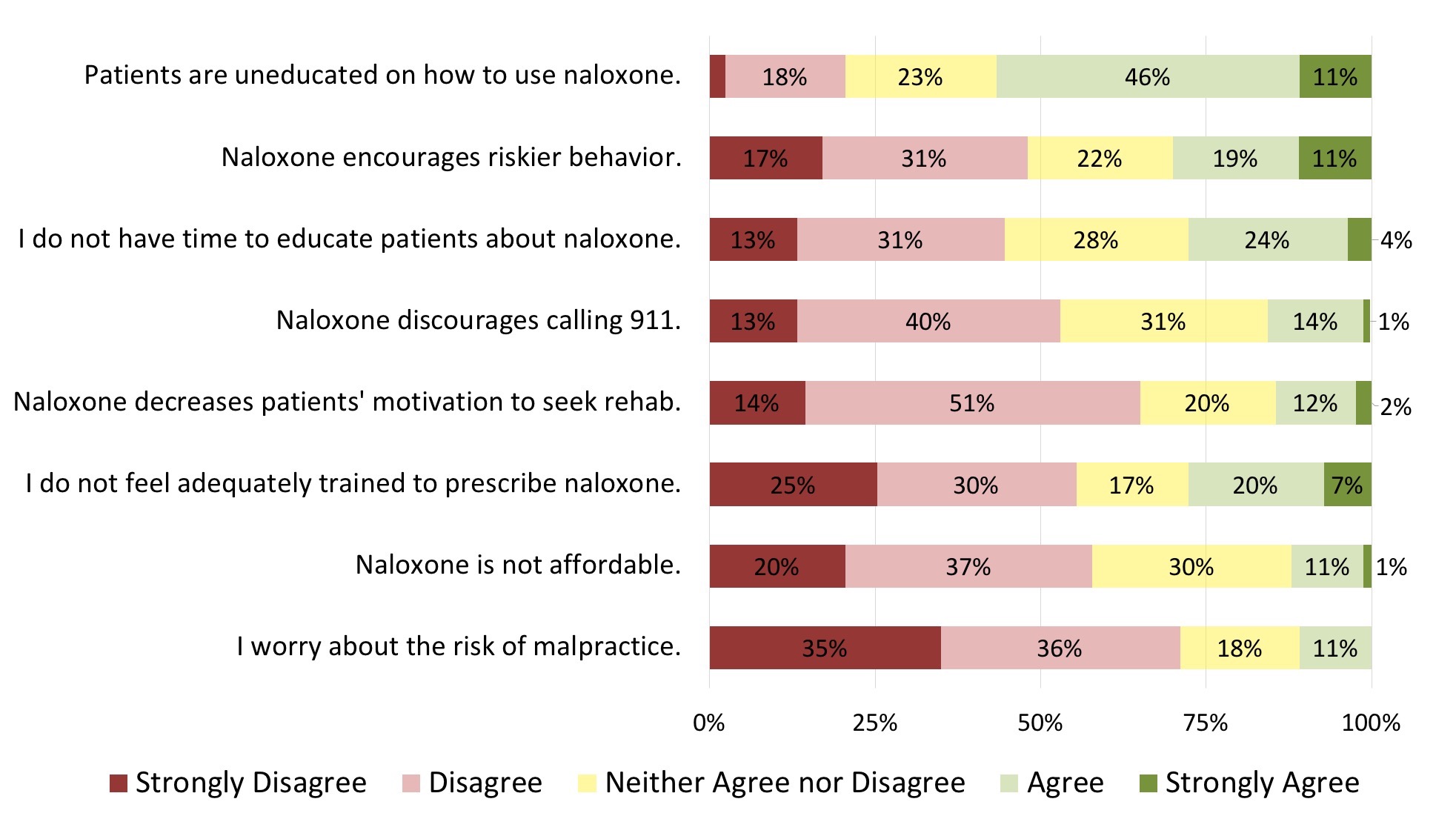
Lack of patient education on proper use of naloxone was the most identified barrier to naloxone prescribing, reported by 57% of respondents. Other identified barriers included potential encouragement of riskier behaviors with naloxone (30%), insufficient time for patient education (28%), and inadequate provider training (27%). Attendings were significantly less likely to perceive adequate time to educate their patients on naloxone use compared to APPs (mean 2.9 vs 1.8, p=0.004). Residents were more likely to report inadequate training to prescribe naloxone to their patients compared to attendings (mean 3.0 vs 2.3, p=0.033).
Conclusions: Overall, hospital providers agree with the CDC recommendations to prescribe naloxone to high-risk patients. However, certain barriers likely affect the rate of naloxone prescribing at hospital discharge, including lack of time, patient education, provider training, and concern for increasing riskier behaviors. These areas can be addressed in future studies to increase prescribing of naloxone to at-risk patients.