Background: The Society of Hospital Medicine identified questioning the necessity of repeat labs in stable patients as a Choosing Wisely goal to improve overall value of care. Implications of unnecessary blood draws include over-testing, pain, decreased patient experience, and risk for iatrogenic anemia. Interventions to safely reduce provider lab orders have been applied in various methodologies and settings. Using “Plan-Do-Study-Act” (PDSA) methodologies, a combination of resident education and encouragement of active discussion about lab orders was implemented with a specific aim to reduce laboratory results on a general medicine team by 0.25 total tests per patient day by January 2018.
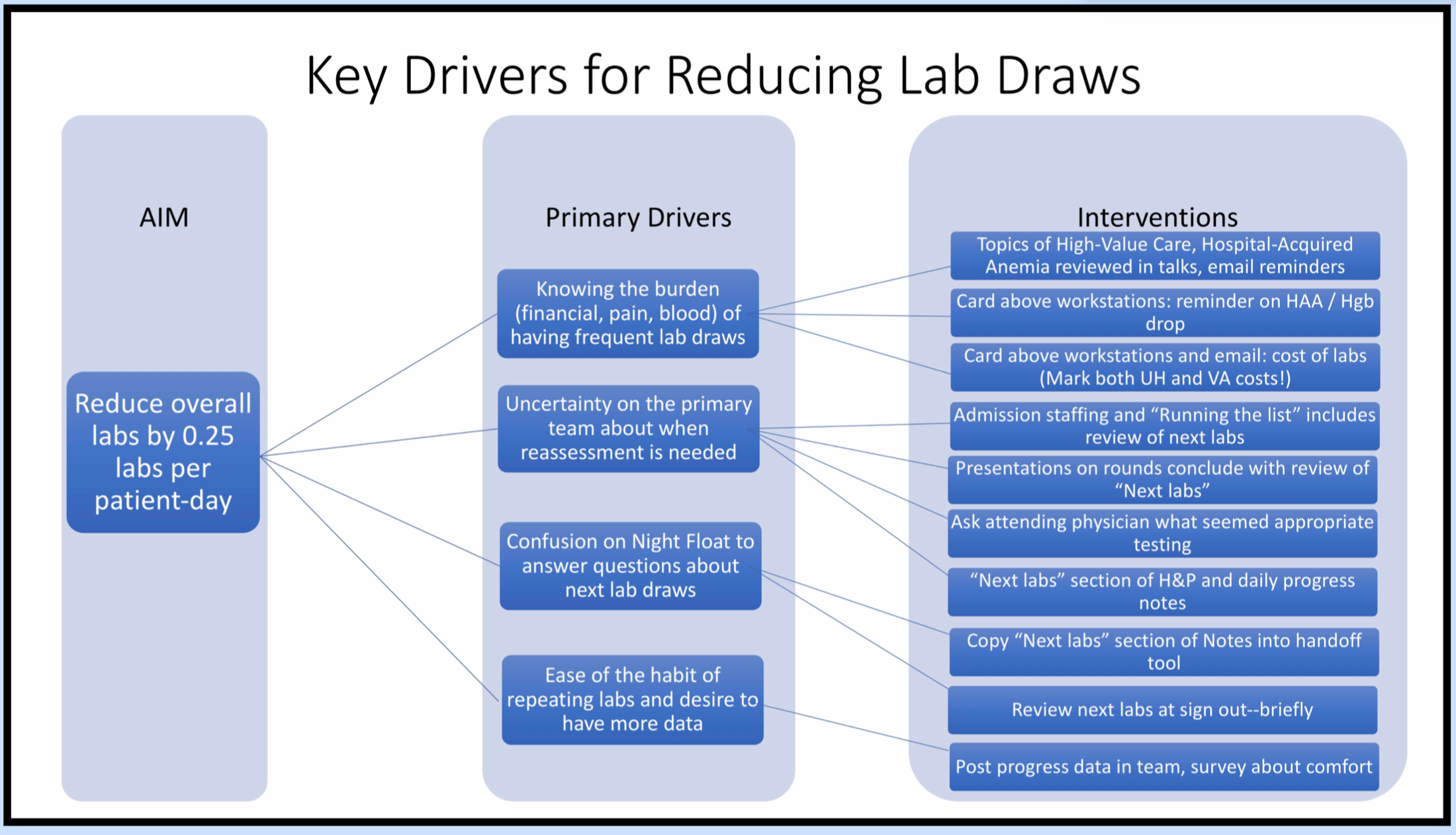
Methods: The first PDSA cycle involved one of four general medicine teaching services at the Louis Stokes Cleveland VAMC. Baseline data was obtained from July 2017 through November 2017. From that time, a multi-faceted intervention was performed at the start of each residency block–and is ongoing. This intervention included an in-person educational session detailing consequences of excessive phlebotomy, an appeal for discussion of laboratory orders during bedside rounds, and a request for addition of a “next labs” section in daily documentation and hand-offs. Reference cards were placed at computer terminals, and an email was sent delineating this information along with a pre-survey for viewpoints on lab ordering practices. A post survey email followed completion of each block. All inpatient ward serum chemistry and CBC tests were collected from a central VA database and analyzed patient-by-patient as total inpatient labs divided by their length of stay, excluding labs obtained while in ICU and cardiac step-down. The mean of these values per block from July 2017 through March 2018 were analyzed using a run chart and pre/post comparisons using t-tests.
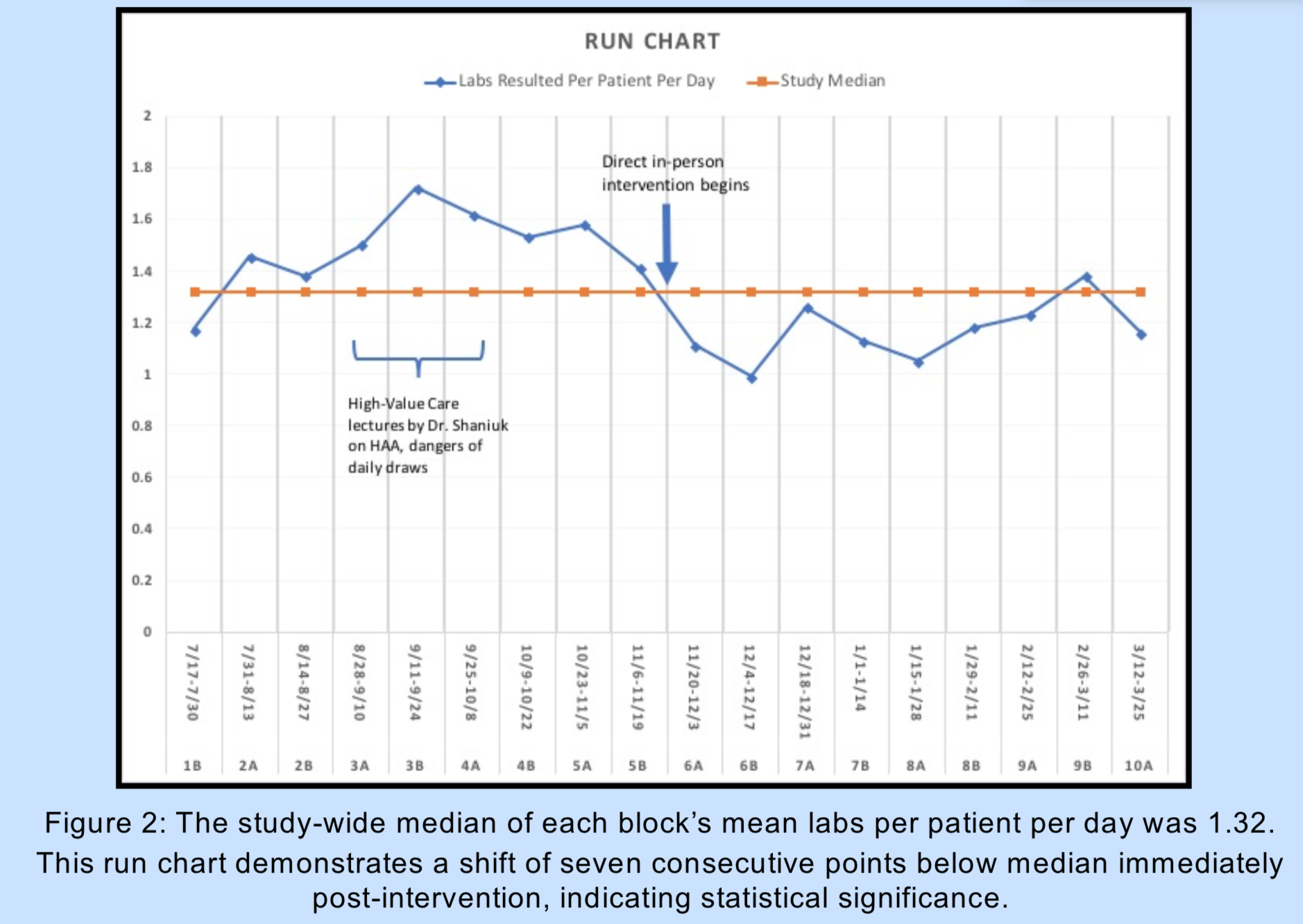
Results: The study-wide median of each block’s mean labs per patient per day was 1.32, with a shift of seven consecutive points below median immediately post-intervention, indicating statistical significance. Early post-intervention data limited to original timeline of Jan 2018 showed significant decrease of 0.38 mean lab results per patient per day from pre-intervention mean of 1.48, (SD=0.16, n=9 blocks) vs post-intervention mean 1.11 (SD=0.10, n=5), (t test p<0.0001). Expanding to all blocks currently analyzed, post-intervention mean is 1.17 (SD=0.12, n=9), (absolute difference 0.319, p=0.0001). Lab result frequency for a given block was not associated to number of patients per block (R=0.162) or length of stay (R=0.257).
Conclusions: Immediately post-intervention, a significant reduction in laboratory tests was observed, and this has continued throughout consecutive blocks. The initial goal of reduction by 0.25 tests per patient per day was achieved and maintained. Future steps include analysis of balance and process measures, controlling for severity of illness, and analysis of PDSA cycle 2 expansion to all four general medicine teams at the VA.