Background: Physicians and nurses often overestimate patients’ understanding of their illness, medications, treatments, and care plans. Fragmented discussions can lead to inconsistent conveyance of key information to patients and their caregivers. Multidisciplinary bedside rounds are an essential opportunity to facilitate patient-centered care. Our medical-surgical units did not have a standardized approach to ensuring consistent, clear communication from a patient’s multidisciplinary team, comprised of physicians, nurses, case managers, social workers, and others. We believed that the lack of ‘face-to-face’ interaction between the full team and the patient led to a downtrend in Patient Experience scores in our medical-surgical unit, as measured through Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS).
Purpose: The purpose of this intervention was to foster multidisciplinary collaboration and ensure patient understanding by requiring standardized communication between the full multidisciplinary care team with patients. To this end, we implemented a communication plan based on the acronym “WE CARE:” 1) Who was present (e.g., who was at bedside in addition to the patient); 2) Everyone on same page (e.g., language and literacy barriers); 3) Connect with patient and family (e.g., promoting patient-centeredness and compassionate care through eye contact, introducing the full team, etc.); 4) Assessing understanding (e.g., explanation of changes to medications, key lab and test results, and post-discharge plans); 5) Response from patient and/or caregivers (e.g., ensuring understanding); 6) Educate/ empathy/ end of conversation.
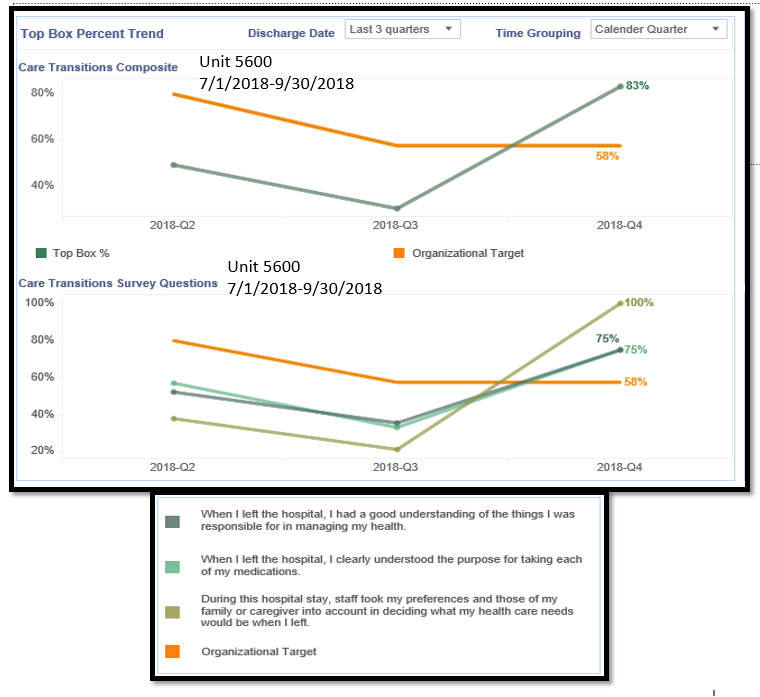
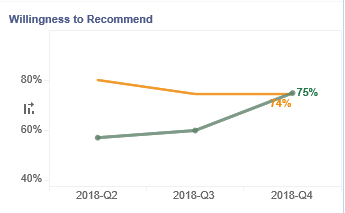
Description: Centered on the WE CARE communication model, we gathered all members of the multidisciplinary care team, e.g., primary nurse, nurse practitioner, social worker, case manager, care transition associate, nurse manager, unit medical director, etc. at a standardized time each day. The full interdisciplinary team would communicate with each patient on the unit at the bedside utilizing the WE CARE model. The intervention was started on one medical-surgical unit on July 2018. We compared our pre-intervention (approximately 63 respondents) and post-intervention (approximately 55 respondents) survey results. In the domain of care transitions, e.g., patient had a good understanding of things patient was responsible for in managing his/her health; patient had a good understanding of purpose of each medication; staff consideration of patient and caregiver preferences post-discharge, there was an increase from 49% in our top-box (an answer of always) composite HCAHPS score to 83%. We also observed an improvement in patient willingness to recommend our hospital, increasing from 57% to 75% for top-box answers, e.g., always recommend.
Conclusions: A focused, structured communication tool, e.g., WE CARE, implemented as a part of daily standardized multidisciplinary bedside rounds led to an improvement in patient satisfaction scores around care transitions and willingness to recommend our hospital.