Case Presentation: A 77 year old male with history of diabetes mellitus, systolic heart failure and morbid obesity who presented with multiple episodes of falls occurring over a 2 week period. The patient reported bilateral weakness and pain in the lower extremities, in addition to sensation of paresthesias and numbness. He reported a progressive loss of ability to ambulate and to maintain balance while standing. He denied back pain, neck pain, fever/chills, weight loss, and other alarm symptoms. Physical exam revealed normal cranial nerve function, preserved upper extremity strength, and reduced proximal hip flexor strength 4-/5. He had diminished sensation bilaterally in the lower extremities. Gait was unsteady and limited. Laboratory work up of suspected peripheral neuropathy included TSH, B12, CPK, aldolase, ANA, LDH, transaminases, anti-SSA/SSB, ANCA, hepatitis serologies, cryoglobulins, acetylcholine receptor antibodies – which were negative.Initially the differential diagnosis included diabetic neuropathy, Guillane-Barre syndrome and others but upon further history the patient reported chronic use of metronidazole prescribed for treatment of chronic diarrhea. The patient reported taking metronidazole 500mg three times daily for a period of approximately 6 months. The cumulative dose of metronidazole taken was around 300 grams.The patient was seen by a Neurology consultant who recommended discontinuation of metronidazole and aggressive physical rehab. The patient was discharged off metronidazole to a skilled nursing facility with outpatient Neurology service follow up.
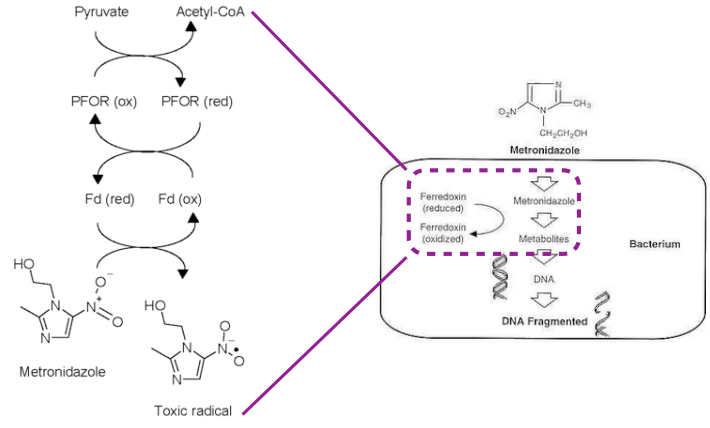
Discussion: Metronidazole, a nitroimidazole antibiotic, used for management of infections due to parasitic and anaerobic bacterial organisms, is widely used in clinical practice. Neurotoxicity related to metronidazole is a well-described but little-known side effect of prolonged use of this medication. Neurotoxicity may involve the central nervous system (CNS) and the peripheral nerves. The overall incidence of this condition is unknown. Patients suffering from metronidazole-induced peripheral neuropathy present with symptoms of a progressive, symmetric distal sensory neuropathy including numbness, paresthesias, and severe pain. The CNS form, known as metronidazole-induced encephalopathy, may present with confusion, ataxia and dysarthria. Metronidazole-induced peripheral neuropathy is more common than the CNS version of the condition, though they may exist concurrently. Metronidazole-induced neurotoxicity is believed to be dose dependent and cumulative with the highest risk occurring at doses exceeding 42 grams. Our patient received 7.5x this amount over a period of 6 months.The pathophysiology of metronidazole induced neurotoxicity is poorly understood. Metronidazole crosses the blood-brain barrier and is believed to cause neuronal oxidation, formation of free radicals and neuronal swelling ultimately leading to neuronal dysfunction and degeneration in animal models.Management includes cessation of the offending drug and aggressive physical rehabilitation. Most patients show improvement in sensory and motor peripheral nerve function after discontinuation of metronidazole therapy.
Conclusions: Metronidazole-induced peripheral neuropathy typically results from cumulative long-term use of metronidazole and may mimic other symmetric, distal peripheral neuropathies. The hospitalist must remain aware of this rare but debilitating complication of metronidazole therapy.