Background: Discharge delays adversely affect patient flow leading to prolonged Emergency Department (ED) boarding time and decrease in hospital bed availability. Discharge improvement processes can mitigate these delays, but in practice it has been difficult to implement and create substantial impact on discharge delays.
Purpose: To develop and implement a discharge physician assistant (DAP) role for the inpatient hospital medicine physician assistant clinical educator (PACE) teams at a large tertiary care hospital, with a goal of earlier patient discharges. A goal was set for DAP patients to have a discharge order placed by 10AM and 80% of DAP patients to have a discharge order before noon.
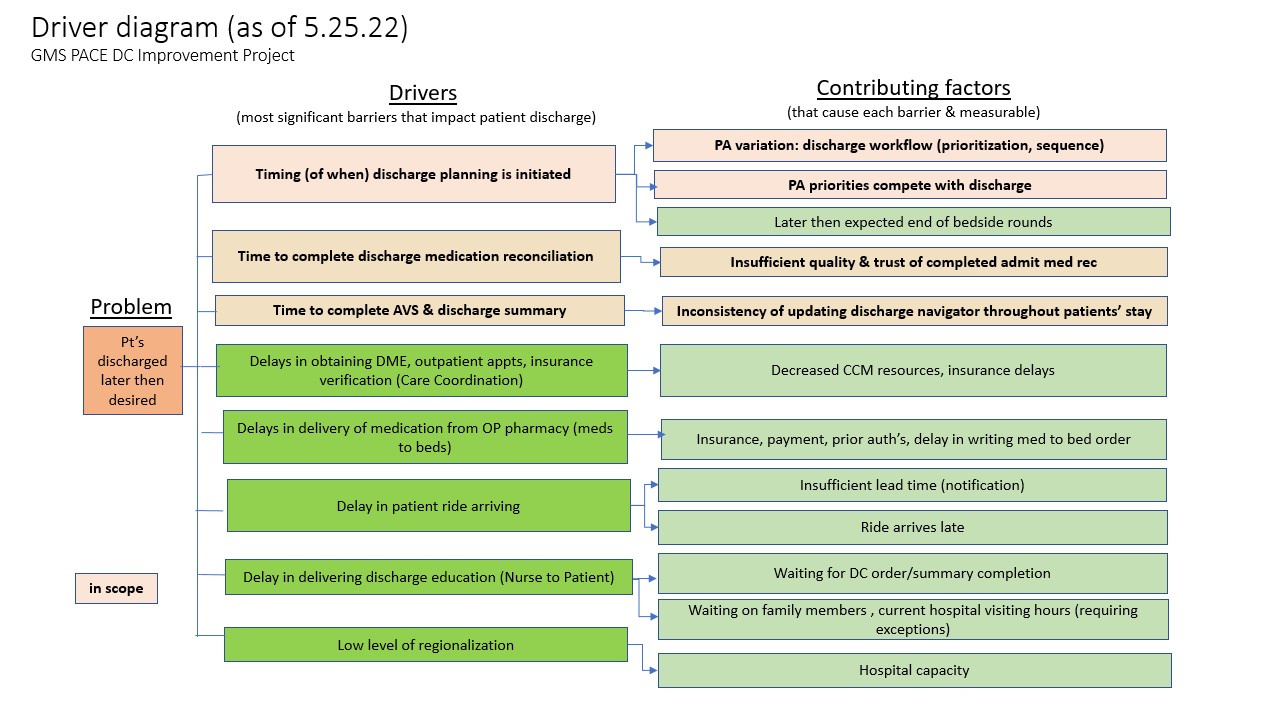
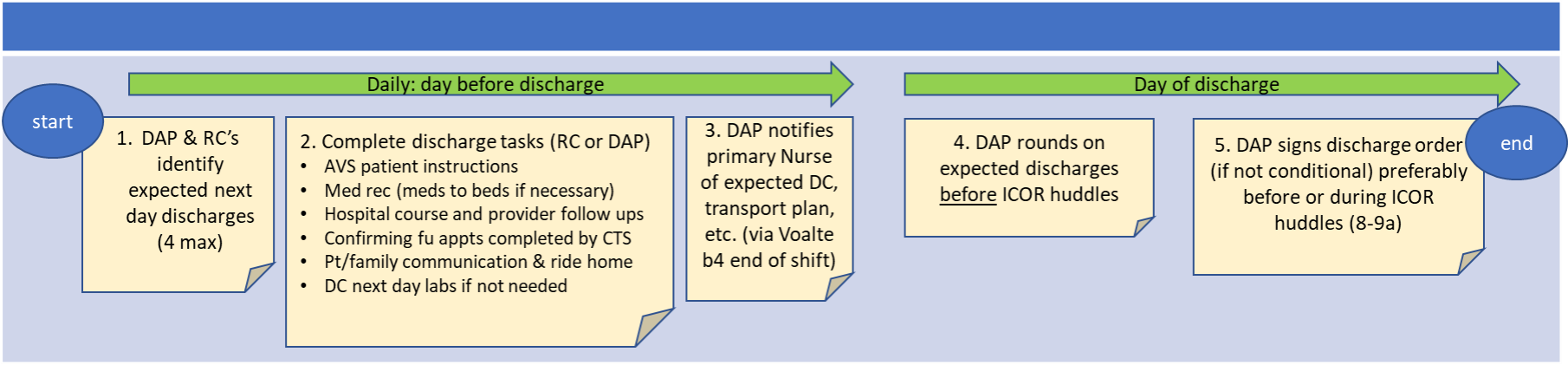
Description: A working group was formed to engage the physician assistants (PAs) that staff the PACE service to identify drivers of discharge delays, and then reviewed to determine which drivers would be within scope for potential solutions (Figure 1). Among all identified drivers there was felt to be an overlying theme of “competing priorities” that impacted discharge timing, including other high importance demands such as daily walk rounds or unanticipated patient instability. Potential solutions were proposed and discussed, with consensus on creation of a Discharge Physician Assistant (DAP) role, with the hypothesis that highly probable discharges could be identified the day prior to discharge. The working group then created a process map of the 24 hours leading up to patient discharge to help determine roles and responsibilities for the DAP (Figure 2), outlining the following roles and responsibilities: (1) On a daily basis, the DAP obtains a list of highly probable discharges for the next day from all 4 teams; (2) the DAP completes preparation of discharge material (e.g., patient instructions, discharge medication reconciliation, confirming ride for the next day); (3) the following morning the DAP assigns themselves as responding clinician, confirms appropriateness for discharge, and completes the discharge process. The DAP pilot was launched in June 2022. Six PAs were selected as DAP champions to initially serve as the DAP and eventually all the PAs were eventually assigned to the DAP role to allow for continued knowledge, and acceptance of the new role and responsibilities. A team performance dashboard was created to monitor rolling median discharge order time, percentage of discharge orders by noon and median discharge time. The dashboard also included a performance scorecard of individual provider discharge practices allowing the opportunity for daily feedback and coaching. During pre-intervention period (October 2018-January 2022), median time of discharge order placement was 1:08pm. In the 5 months since the DAP launch, DAP discharges account for 20-30% of total team discharges and the median time of discharge order placement is 9:07am, with 100% of DAP patients achieving placement of discharge order before noon.
Conclusions: Creating a discharge role responsible for discharge preparation the day before discharge and completion of discharge the next morning has been successful in reducing the median time for discharge order placement and achieving 100% discharge order before noon. The DAP additionally allows the other team providers time to focus on patients who are not medically ready for discharge. Next steps include collecting additional data, including nursing notification of discharges, nurse hand-off and identifying barriers that would impact discharge time.