Background: Co-managed care models have become increasingly popular as a result of their positive impact on patient care. This has been seen through improvement in quality metrics such as readmission, LOS, and adherence to evidence-based care pathways. Surgical hospitalist models have paved the way for new collaborative models that standardize care and optimize inter-specialty communication. Cardiology patients, historically, represent the largest portion of inpatients with well-defined evidence-based standards that have a disproportionate impact on outcome-driven incentives. Traditionally, both academic and non-academic centers have employed either consultative cardiology service lines under the direct care of numerous hospitalists or, less often, a primary cardiology service overseen by a Cardiology Attending.
Purpose: In this presentation, we will walkthrough how our multidisciplinary team developed a novel hospital medicine-cardiology co-management service line to optimize care of telemetry patients and significantly enhance Internal Medicine resident and Cardiology Fellow education. From the perspectives of both hospitalists and cardiologists, we will explore discrete opportunities for enhanced patient care through a co-management model while problem-solving barriers to its implementation and sustainability.
Description: The Cardiology inpatient medicine team consists of a hospital medicine attending, IM residents, Intern residents, and a dedicated “teaching” cardiologist. Patients are triaged and cohorted to maximize the volume of shared patients between the hospital medicine team and the dedicated cardiologist. This geo-localized collaborative system permits optimal communication between services through a novel hybrid rounding structure. The Cardiologist takes a unique role in this model by reviewing clinical and diagnostic data directly with the residents and providing high yield Cardiology didactics. These complementary roles create a close working relationship between teams while allowing each service to work within scope and strengths.
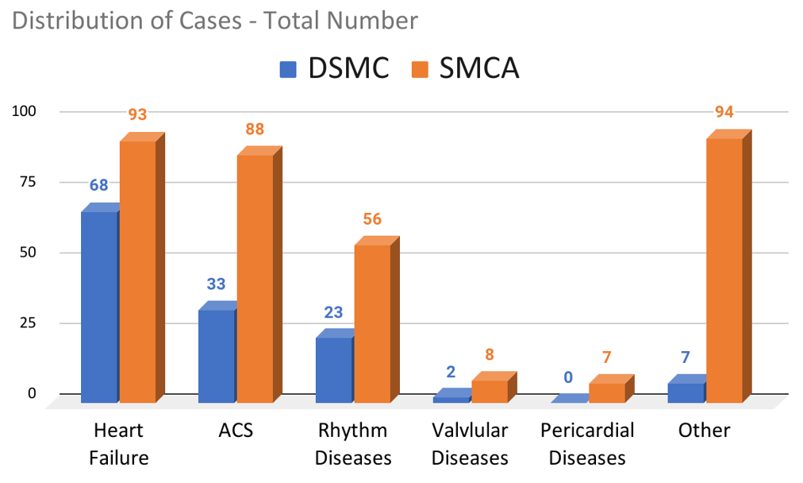
Conclusions: Our Cardiology-Hospitalist Co-management model has been impactful in several ways. Adherence to cardiology care standards such as heart failure protocols, consultation appropriateness, collaborative heart failure readmission work, and advance directive planning for heart failure patients are apparent. Early returns in resident cardiology education are noteworthy including an average 10-fold increase in resident cardiology diagnosis exposure as well as improved cardiology ITE scores. Lastly, cardiologist and hospital medicine experiences with this model were explored using thematic analysis. The feedback was overwhelmingly positive with respondents indicating that this model was elegant and easily applicable.