Background: Clinical decision support tools based on predictive analytics can provide actionable information and improve clinical outcomes for patients at risk of developing sepsis. Scoring systems such as Systemic Inflammatory Response Syndrome (SIRS) and National Early Warning Score (NEWS) that were not specifically trained to detect sepsis tend to have high false alarm rates, leading to physician alarm fatigue. Our academic institution previously implemented NEWS to prompt assessment for sepsis, but 63% of alarms were cancelled by the care nurse. The goal of this study was to develop a machine learning model to improve early detection of sepsis, leveraging state-of-the-art deep learning.
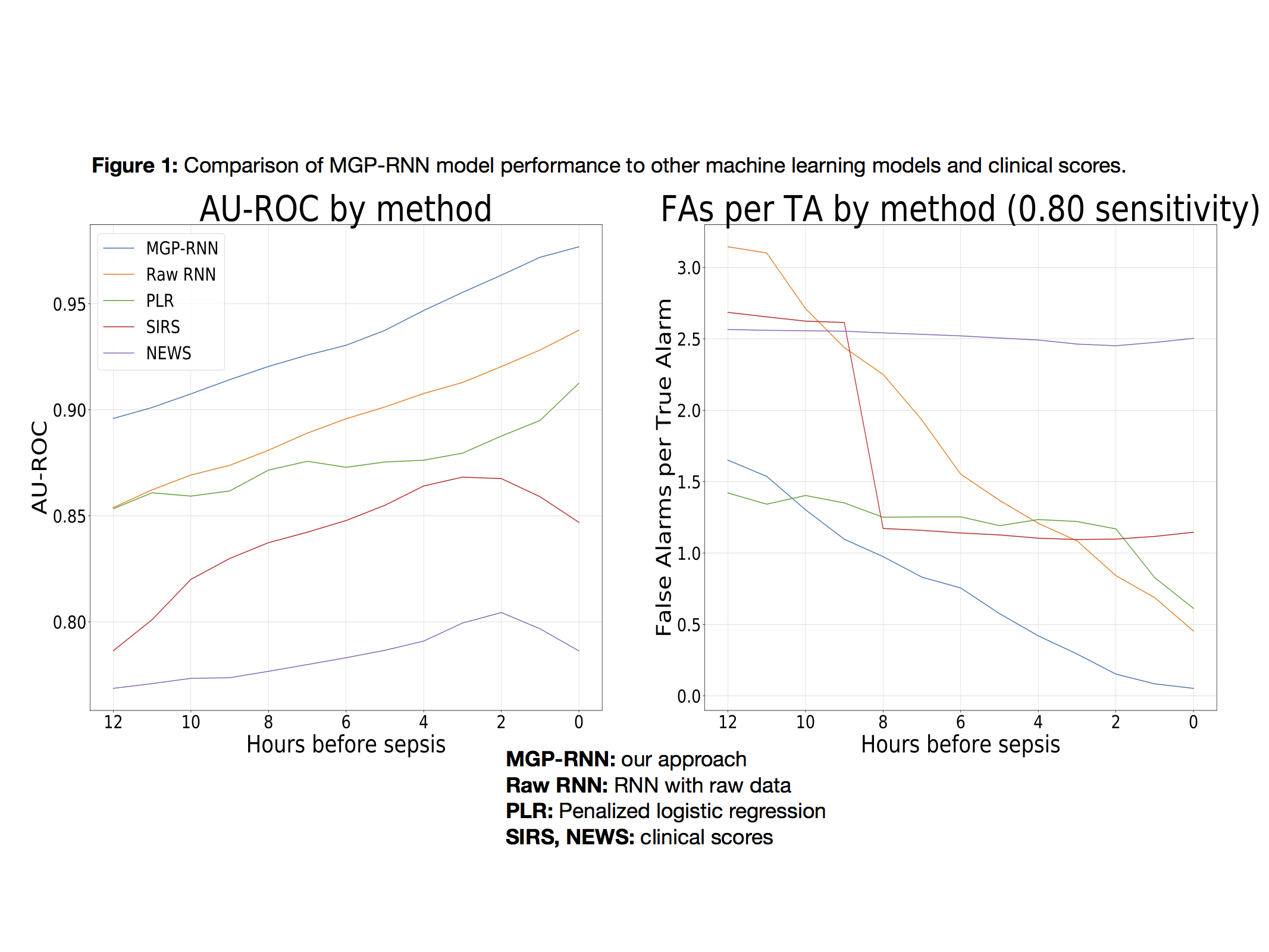
Methods: This was a retrospective study of all adult inpatient admissions (n=43,046) at a large academic hospital from October 1, 2014 to December 31, 2015. Patient demographics, comorbidities, vitals, lab results, and medication data were extracted from the electronic health record (EHR), yielding 83 predictor variables. Our dataset included 25 million vital sign measurements, 1.9 million medication administrations, and 5.2 million lab results. We used deep recurrent neural networks (RNNs), a form of deep learning for sequential data, to predict onset of sepsis. We combined this deep learning model with multi-output Gaussian processes (MGPs), which interpolate and impute continuous functions for physiological time series variables, to create our final model, denoted MGP-RNN. We compared MGP-RNN with a RNN (“Raw RNN”), penalized logistic regression (PLR), SIRS, and NEWS. We calculated C-statistics and false alarms per true alarm at 80% sensitivity, as a function of the number of hours in advance of sepsis.
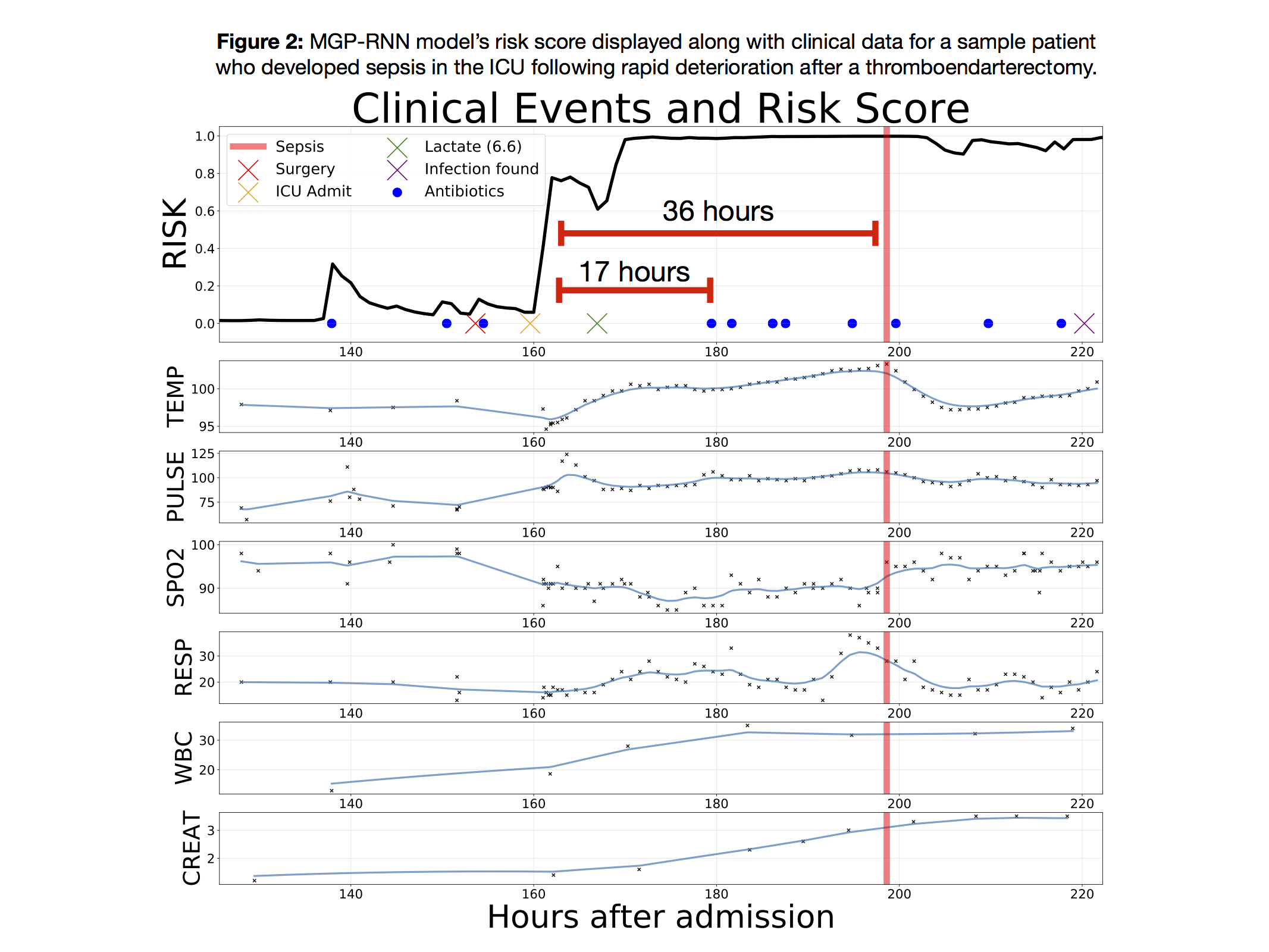
Results: Figure 1 compares performance among machine learning models and clinical scores. Our proposed MGP-RNN consistently performs best, both in terms of C-statistics and false alarms. The machine learning methods generally perform better than the clinical scores, and NEWS performed worst overall. Figure 2 demonstrates an inpatient timeline for a sample patient; our model detected sepsis 17 hours prior to the first antibiotic administration for infection and 36 hours before a sepsis definition was met.
Conclusions: In this study, we developed a deep learning approach to improve early detection of sepsis. Our model consistently outperformed strong baseline methods, and had considerably fewer false alarms than SIRS and NEWS. Our methodology ingests commonly available predictors from the EHR and can be applied to predict other inpatient events, such as cardiogenic shock, cardiopulmonary arrest, and mortality.