Background: Although central line-associated bloodstream infection (CLABSI) rates are publicly reported, whether these data correlate to clinical documentation or practice is not known. Using data from a large hospital collaborative, we hypothesized that physician documentation and blood culture rates among patients with peripherally inserted central catheters (PICCs) would be associated with standardized infection ratios (SIRs).
Methods: Data from the Michigan Hospital Medicine Safety (HMS) Consortium, a 47-member Blue Cross Blue Shield-of Michigan funded collaborative, was used for this analysis. Trained abstractors reviewed patient medical records for the following: NHSN-defined CLABSI events (modified to exclude determination of “infection at another site”); physician documentation of CLABSI; an order for PICC removal for confirmed or suspected infection; documentation of “line sepsis,” or “line bacteremia,” and numbers of blood culture ordered. Event rates at each hospital were summarized as the number of events per 1000 catheter days. SIR data for each hospital was obtained through the National Healthcare Safety Network (NHSN) database with hospitals stratified by SIR rates (<1 or >1). Association between documentation, blood culture rates, hospital factors (e.g., bed size) and SIR were assessed.
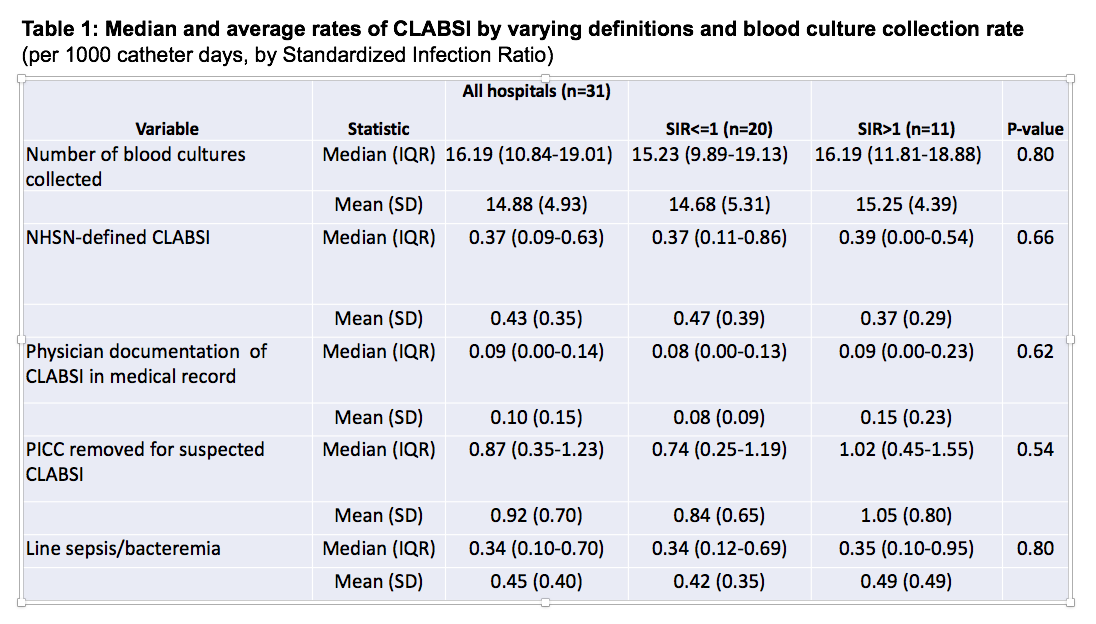
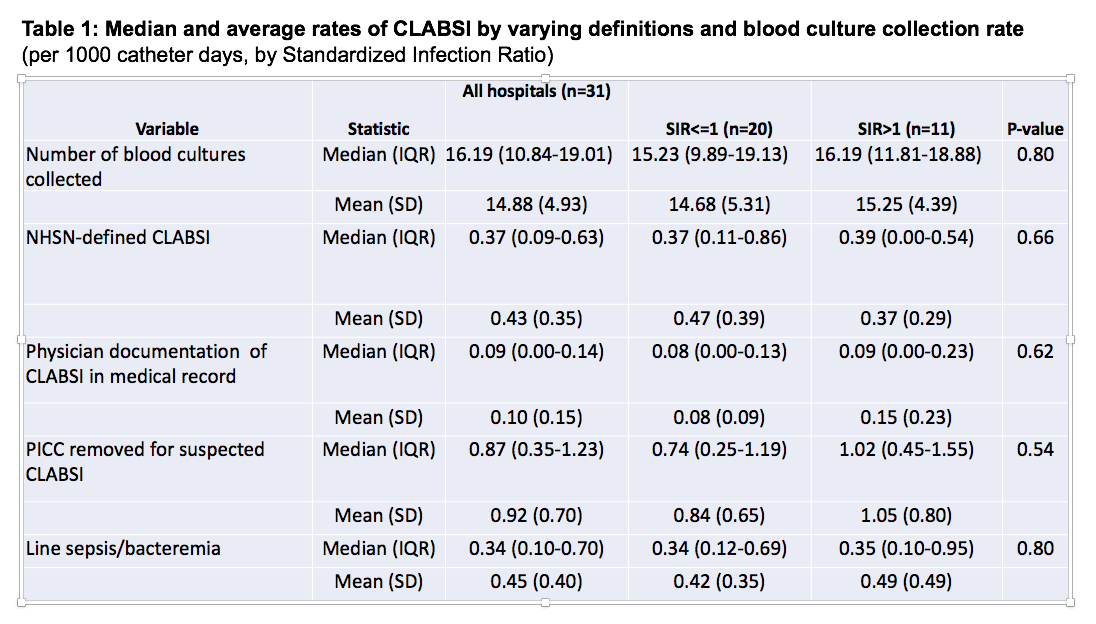
Results: Data from 31 of 47 HMS hospitals (66%) was available and included in the analysis. Substantial variation in numbers of blood culture performed (median=16.19 [IQR=10.84-19.01]) NHSN-defined CLABSI events (median=0.37 [IQR=0.09-0.63]) physician documentation of CLABSI (median=0.09 [IQR=0.00-0.14]), PICC removal for suspected or confirmed CLABSI (median=0.87 [IQR=0.35-1.23]) and documentation of line sepsis or bacteremia (median=0.34 [IQR=0.10-0.70]) was noted across hospitals (Table 1). No association between any individual category and hospital SIR was noted. Similarly, when analysis was stratified by SIR, no associations between practices and documentation were observed (p>0.05 for all measures). The number of blood cultures ordered was not significantly associated with SIR. Hospital factors such as bed-size, for-profit or academic status and length of patient stay were also not significantly associated with SIR (Table 2).
Conclusions: In this analysis of hospitalized patients with PICCs, publicly-reported rates of infection do not correlate with physician documentation, blood culture orders or key hospital characteristics. Future studies to better understand drivers of this discrepancy appear necessary.