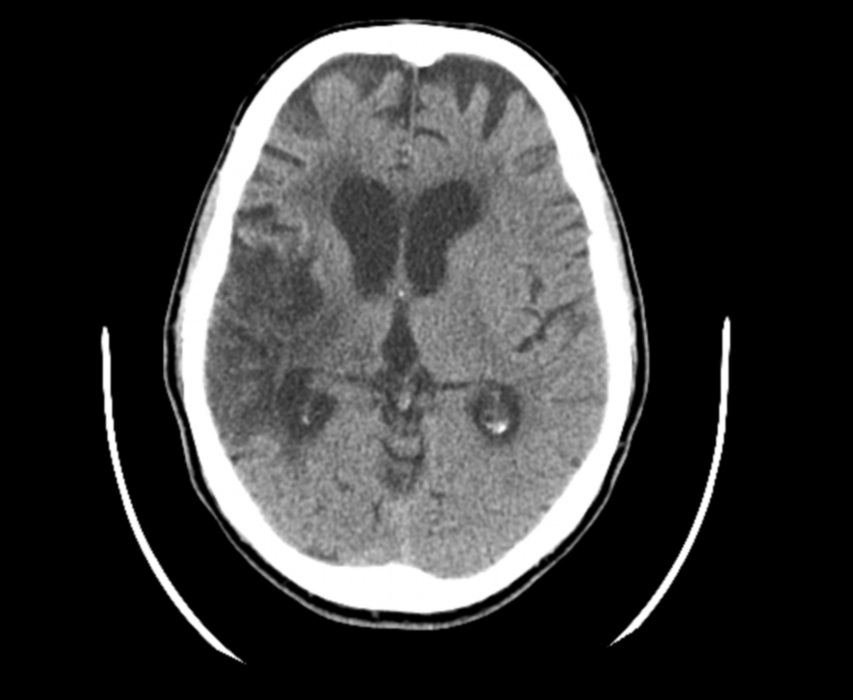
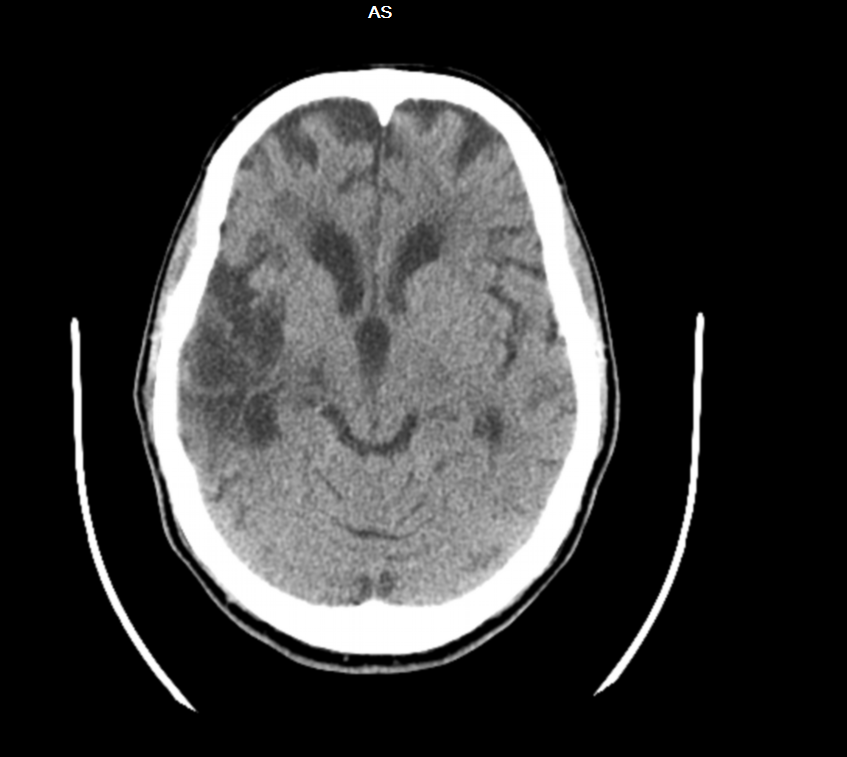
Case Presentation: Dejerine-Roussy syndrome is a rare condition usually caused by ischemic or hemorrhagic strokes involving the thalamus. Patients develop dysesthesia or allodynia, weeks to months after the initial stroke. We present a case of central thalamic pain in a patient who presented with a middle cerebral artery (MCA) infarct with thalamic involvement. A 77 year old female presented to the emergency department for an episode of syncope and left upper and lower extremity pain. The pain was sharp, burning, and 5/10 intensity on a numeric scale of 0 to 10. She noted sweating prior to the syncope, which lasted for less than 5 minutes. No associated convulsions, incontinence or tongue bites were reported. She had a history of paroxysmal atrial fibrillation on Apixaban, prior CVA with residual left hemiplegia, and peripheral vascular disease. Physical examination revealed left sided spastic hemiparesis, positive left Babinski’s, left homonymous hemianopia and left sided allodynia. CT brain was suggestive of an old cerebral infarct in the right MCA territory, involving the right temporal and parietal lobes, with involvement of the right thalamus and brain stem. MRI showed acute large right sub cortical and left brain stem hyper intensities extending to the thalamus. Small left subcortical hyper intensities were also noted. The allodynia was interpreted in the context of Dejerine-Roussy thalamic central pain syndrome. The patient was started on Pregabalin and physical therapy, with considerable improvement.
Discussion: Central pain syndrome is estimated to affect 5-10% of patient with CVA, the incidence being higher in patients over the age of 85 years. The thalamus is the relay center for the somatosensory pathway, and any lesion disrupting the spinothalamic tract through its course, including subcortical, capsular, lower brain stem and lateral medulla, can stimulate the symptoms of Dejerine-Roussy syndrome. Although an ischemic event precedes most central post-stroke pain, the pain can also happen after hemorrhagic stroke. The central post-stroke pain occurs more frequently in those with acute stroke and larger lesions. Frequently the symptoms start within the first 6 months of stroke, but can develop even 10 years after infarction. The management of central post-stroke pain requires a multidisciplinary approach and includes antidepressants, anticonvulsants, opioids, N-methyl D-aspartate receptor antagonists, and non-pharmacological options. Other therapies considered in refractory cases include, TENS, motor cortex stimulation and deep brain stimulation. If antidepressants and anticonvulsants are not effective alone or in combination, opioids may be considered. Intravenously-infused tramadol can be effective in patients with severe central poststroke pain.
Conclusions: With an ageing population, this may become a more frequently encountered condition. Early diagnosis and treatment can alleviate pain and improve the quality of life.