Background: Delirium is a common complication within the hospital setting with nearly one in three older patients experiencing it during hospitalization. Reduction in delirium is associated with decreased falls, decreased distress of patients and caregivers, and decreased length of stay as a result. Identification and reduction of delirium, therefore, is of the utmost importance to the field of hospital medicine.
Purpose: We incorporated a scoring system to identify patients with delirium while hospitalized. With appropriate identification of these patients, effectiveness of interventions can then be evaluated objectively. Ideally, reduction in delirium prevalence across a patient population would be the leading metric and result in improvement for lagging metrics such as length of stay or patient satisfaction.
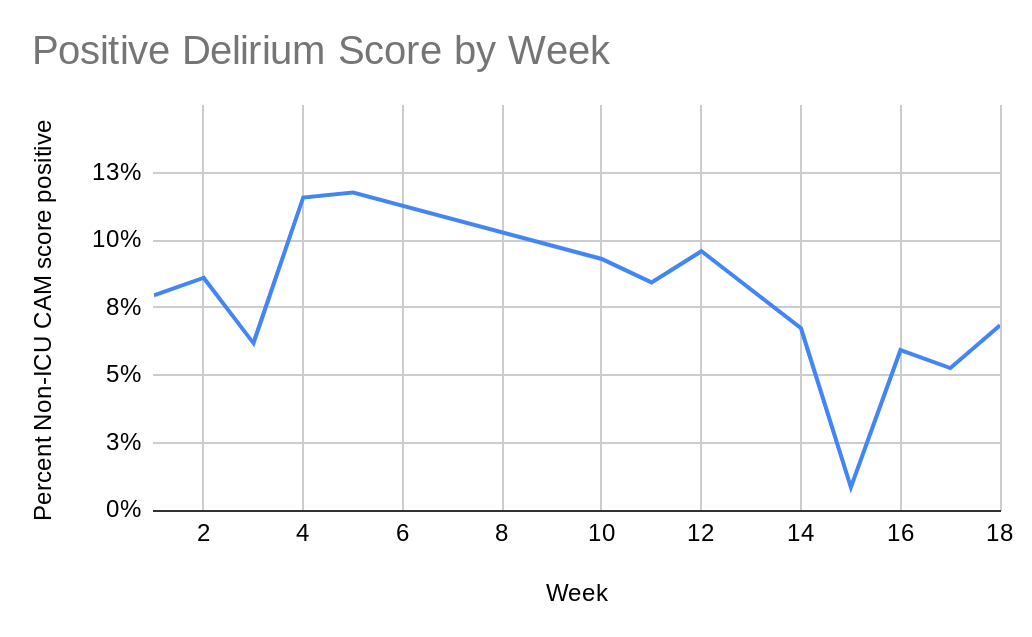
Description: Over a five month period, we incorporated a delirium scoring system throughout our intermediate care (step-down) patients. A CAM (Confusion Assessment Method) score is already commonly used within the ICU setting and the same training was used to teach nurses within the step-down how to screen patients. This was labeled as a non-ICU CAM score and a patient would either score negative (zero) to indicate no delirium present or positive (one or greater) to indicate the patient currently had delirium.Once a patient was screened to have delirium, a pharmacist was notified to review medications and recommend changes to reduce delirium. Physicians were advised to avoid medications known to increase risk to delirium (i.e. benzodiazepines, opiates) and medications were re-timed as to avoid waking patients in the middle of the night if possible. This intervention led to an average decrease in positive non-ICU CAM score of around 10.5% down to near 8%.Further interventions included discussion with nursing to encourage good day and night cycles. This included blinds open and lights on during the day along with blinds closed, lights off, sounds and vital signs minimized at night. Physicians were encouraged to avoid use of bedrest orders, replacing them with up to chair for meals orders. These interventions were encouraged as long as the clinical scenario allowed for continued safe patient care. A flyer was distributed among nurses while the main points of this flyer and the interventions were discussed frequently during the daily nursing huddle by the physician. Based on the initial results of the non-ICU CAM score, it was found that over 10% of patients on the step down service were scoring positive for delirium. After the pharmacy medication review, the delirium positivity score decreased from over 10% down to near 8%. The further interventions with nursing and physician education led to a further decrease in delirium positivity near 5%. Overall, our cumulative interventions decreased patients with delirium in half from near 10% to 5%.
Conclusions: We developed a system for detection of patients with delirium and incorporated interventions to reduce the prevalence of delirium. Initial testing indicates significant delirium reduction with pharmacy medication review, nursing education, and physician education. Further research would be beneficial to assess the correlation with length of stay and mortality.