Background: At our urban, academic hospital, use of outdated protocols and unnecessary variations in the care of DKA patients treated with ICU requiring IV insulin protocols have led to multiple safety events, delays in care with associated increased costs, and overtreatment of hyperglycemia with ketosis frequently resulting in unnecessary ICU utilization. After multi-disciplinary stakeholder development and adaptation of the 2009 ADA DKA guidelines, we implemented a DKA evaluation and management pathway on 11/7/2016 for use in all hospital units via a centralized pathways web and mobile accessible collaboration platform, with an aim to reduce inpatient ICU utilization and overall length of stay (LOS).
Methods: We conducted a retrospective, single-center pre-post analysis of disposition and LOS for DKA patients ≥18 years old presenting to our ED who met DKA criteria pre- (11/7/2015-11/6/2016) and post- (11/7/2016-8/6/2017) implementation of the pathway. In February 2017, our ED also operationalized a 5 bed critical care resuscitation unit to optimize the care of patients needing temporary critical care resources. Pre-post implementation Chi-squared analyses were performed to assess for change in hospital resource utilization and mean LOS was analyzed using paired t-test with p-values <0.05 considered statistically significant and corresponding 95% confidence intervals reported.
Results: 133 and 120 patients were treated pre- and post-implementation respectively. Pre-post implementation comparisons are presented in Table 1. Significant findings include decreased ICU disposition (66.9 vs 37.5%, p<0.0001) and decreased transfers to other health system hospitals due to bed constraints (23.3 vs 7.5%, p<0.001). ED LOS was longer in the post-implementation period (10.3 vs 13.3 hr, p<0.01) without a significant change in overall hospital LOS. The pathway averaged 141 unique views per month following dissemination and was the most viewed pathway among nearly 160 total pathways.
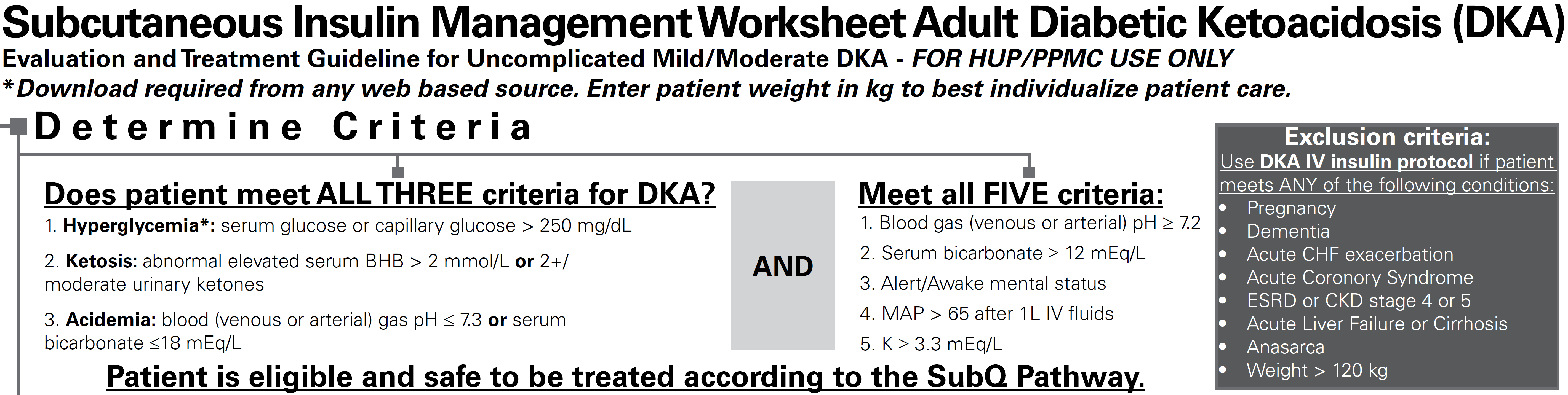
Utilizing a real-time electronic alert system and dashboard, we performed rapid cycle interventions to iteratively refine the pathway. Preliminary findings led to the implementation of a subcutaneous (SC) insulin pathway for eligible patients with mild to moderate DKA beginning February 19, 2017 (Figure 1). Utilizing real-time text message alerts to notify providers of eligible patients, the SC pathway was opted-in among 17 of 39 eligible patients (43.6%). A significant decrease in ICU utilization was found among SC pathway treated patients (0 of 17 patients) compared to those eligible for the SC pathway but treated with the IV pathway (8 of 22 patients, 36.4%, p<0.01).
Conclusions: Our multi-disciplinary implementation of adapted, evidence-based DKA pathways was associated with a reduced need for inpatient ICU utilization without a significant change in overall LOS. Future directions will necessitate electronic clinical decision support to enhance pathway uptake, facilitate sustained high value care, and promote dissemination of these pathways more widely.
.png)