Background: This is an exciting time for Telemedicine with new programs being implemented across the continuum of care including acute care, post-acute care, and in home settings. Proving the value of telemedicine programs when no access to providers exist is relatively straightforward but proving value of programs where implemented to augment existing care by the same specialty is challenging.
Purpose: While several Tele Hospitalist programs currently exist, the vast majority are directed where bedside hospitalists are not available. We postulated a multifaceted role for Tele Hospitalist at busy tertiary centers in improving ED throughput and efficiency of the bedside Hospitalist team as well as enhancing resident education and training in Medicine.
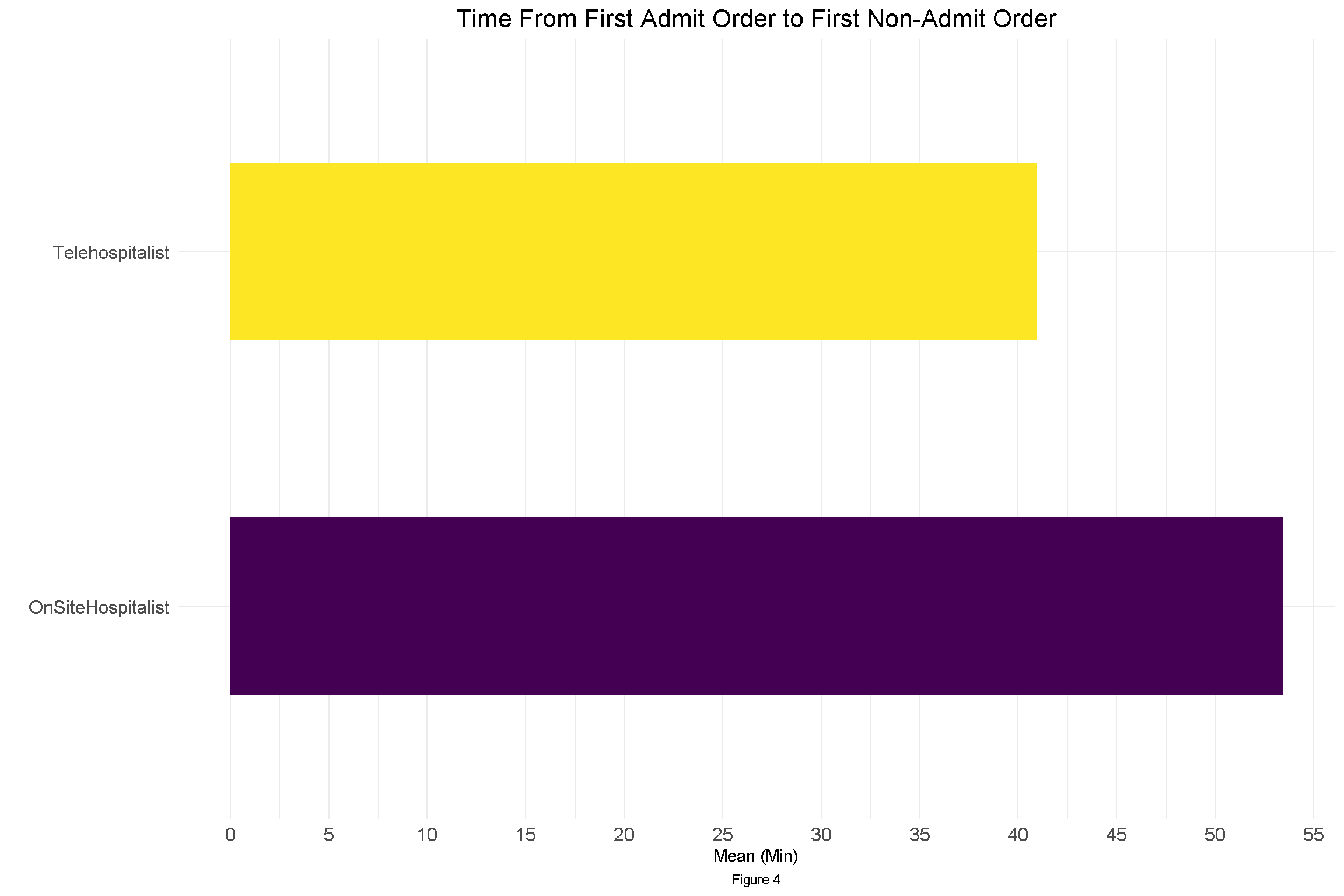
Description: Northwell Health is the largest health system and private employer in the state of New York with over 23 hospitals and over 10.000 physicians. The Tele Hospitalist program was launched to evaluate patients in the Emergency Department (ED) of two tertiary hospitals with the greatest need for improvement in the ED throughput. The program was staffed by employed hospitalists working from the Tele Health hub. The program is staffed by one Tele Hospitalist from the hours of 12pm to 10 pm, seven days a week and was supported by ancillary staff at the center. When the bedside Hospitalist anticipate a delay of over 30 minutes in evaluating a patient after ED notification, they have the option to request a Tele hospitalist consult. Once the Tele hospitalist receive the patient information, they evaluate the patient via a mobile cart. After reviewing their labs and radiology, they performe a full admission including medication reconciliation, consult note, and sign out to the bedside hospitalist. In the evening hours, the Tele hospitalists evaluate patients together with the Family Medicine residents, providing feedback and education. This additional function performed by Tele hospitalists has gained recognition as a valuable benefit for the teaching service by the residency program. Evaluation of 10 month data from site with higher volume demonstrated the following: 1. Total of 3743 patients were evaluated by the bedside hospitalist compared to 644 by the Tele hospitalist in the hours of 12-10PM. 2. Mean Charlson Comorbidity index was 4.54 for the patients evaluated by the bedside hospitalists versus 4.41 for the patients evaluated by the Tele hospitalist, demonstrating that there was minimal difference in severity of illness of patients seen by the two groups. 3. There was almost no difference in the mean age between the two groups of patients, 66.9 years for bedside hospitalists versus 67.7 years for the Tele hospitalists. 4. The visits where the patient was seen by Tele hospitalists showed a decrease in time between first admit order (by ED) and second admit order (by hospitalist) by 13 minutes (p < 0.01), See Graph 1. A similar decrease of 12.5 minutes (p<0.01) was seen between the two groups when examining the time between the first admit order (by ED) and the first non-admit order. 5. Overall high distribution of patient satisfaction based on surveys sent to patients seen by the Tele hospitalist service.
Conclusions: We demonstrate value for the Tele Hospitalist program at a tertiary center for offloading the workload of the bedside hospitalist during busy hours, as well as for patient satisfaction and resident education.
With expansion of the program to step down units, medical floors and skilled nursing facility we plan to develop a multifaceted role for the Tele Hospitalists .