Background: Discharge to post-acute care settings (PACs), such as skilled nursing facilities (SNFs), requires significant, complex discharge planning which often needs to be started early during hospitalization to be complete by time of discharge. This study sought to identify and model factors which predict a given patient’s likelihood of requiring PAC after discharge, using routinely collected electronic health record (EHMR) data available within 24 hours of admission.
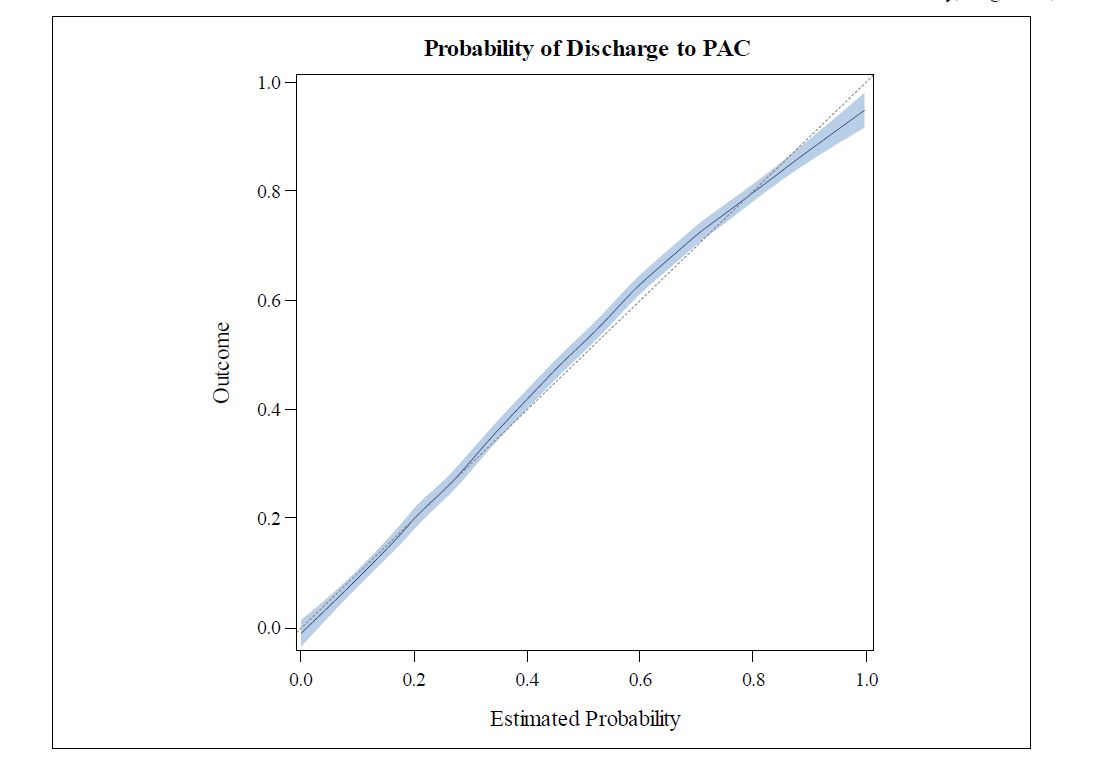
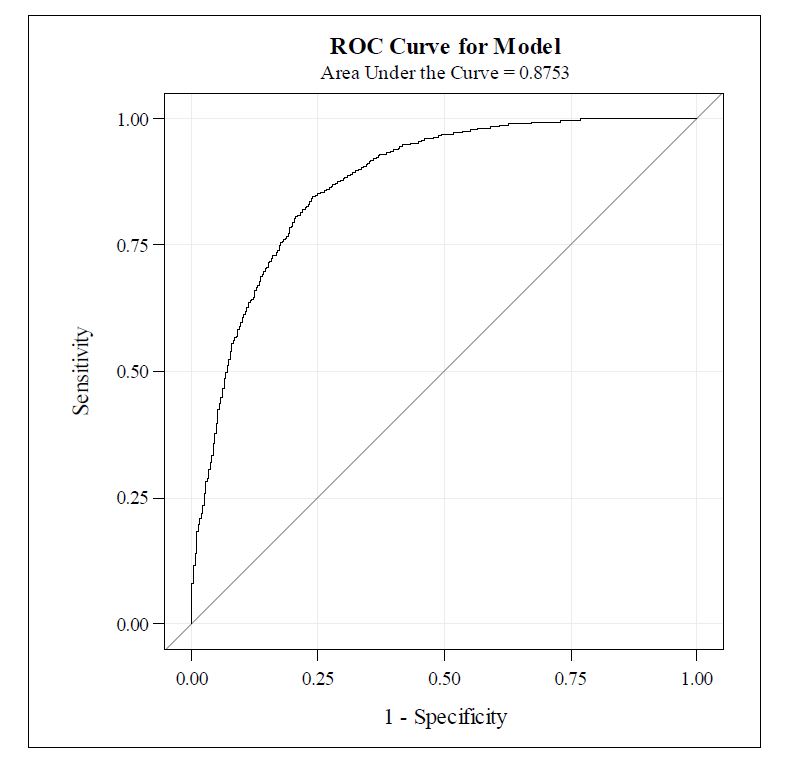
Methods: We performed a retrospective observational study, using data cataloged in the Vanderbilt’s Perioperative Data Warehouse (PDW). We studied adult patients at Vanderbilt University Medical Center whose discharge destination could be identified between September 1, 2017 to August 1, 2018. Variables included demographic, clinical, and laboratory data collected within 24 hours of admission. In addition, we also incorporated commonly used nursing data such as the Morse Fall Risk score and Braden Skin Breakdown score into our analysis, as these might be early predictors of which patients will require nursing services after discharge. We performed logistic regression to derive a model from a subset of the available records, which were under-sampled to account for the large ratio of discharges to home versus discharges to PAC. We generated a calibration plot to assess goodness of fit and outliers. We assessed for potential collinearity using Eigenvalues and variance inflation factor values . We validated the model using a holdout data set of 2000 observations. We report model performance with the ROC plot (discrimination) and a matrix comparing observed with predicted discharge disposition (calibration).
Results: Clinical, nonclinical, and demographic data were retrieved for 6000 eligible admissions. Odds ratios showed that patients admitted to the intensive care unit (1.51, 95% CI 1.50-1.27) and admission from the emergency department (1.53, 95% CI 1.31-1.78) had higher odds of admission to a PAC facility than those who were not. Those who were older (1.0, 95% CI 1.03-1.04), took more home medications (1.06, 95% CI 1.31-1.78), and higher fall risk scores at admission (1.03, 95% CI 1.02-1.03) were also somewhat more likely to experience that outcome. Model calibration via visual inspection was outstanding in the validation set. The regression model showed that probability of discharge to PAC is well correlated to the obtained score from the prediction tool. Overall, the model predicted the correct discharge destination in 81.2% of the calibration cases (Figure 1). The receiver-operator curve plot showed that the area under the curve was 0.875, where 1 represents the perfect predictive tool (Figure 2).
Conclusions: A model that utilizes laboratory data, clinical factors, and functional assessments has outstanding model performance in predicting discharge to a post-acute care facility.