Background: Appropriate use of consultation can improve mortality and decrease cost of care. However, inappropriate consultation may carry risks to patients. Little is known about the variability of inpatient consultation. We aim to describe patient-, admission-, and physician- level factors that influence the variability of inpatient consultation.
Methods: We conducted a secondary analysis of 2011-2015 data from the University of Chicago Hospitalist Project, an existing study using interviews, administrative records, chart review and physician surveys (including questions about practice patterns, burnout, and career plans) to assess care of hospitalized patients. Admissions with LOS≤5 days were included to minimize attending hand-offs. The primary outcome was number of consults per admission, defined by counting the number of unique services that wrote notes minus the primary team. Patient (age, gender, payor) and admission characteristics (year, LOS, teaching service) were obtained from administrative records. Physician characteristics (years in practice, gender, hospitalist or subspecialist, survey results) were obtained from public resources and Hospitalist Project data. To determine factors associated with consultation variability, bivariate linear regressions were used as a basis for multivariable regression models clustering on attending.
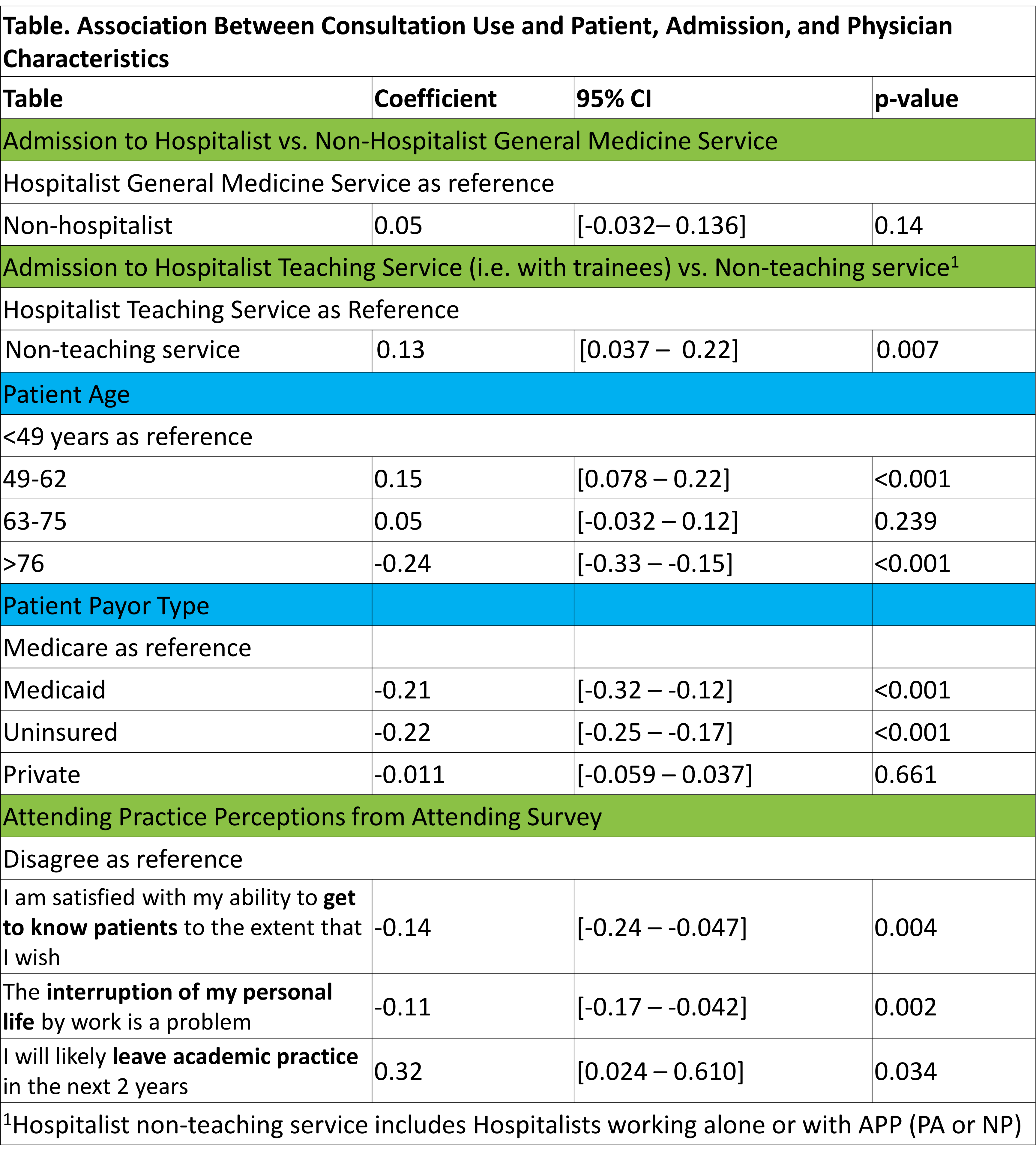
Results: 28,438 General Medicine admissions were included. 632 attendings were included; 37.8% were female and average years of practice was 20.7 years (SD=11.5). 13,770 patients were included; 57.4% were female and mean age was 61.1 years (SD=18.9). The median number of consults per admission was 1 (IQR=1). Consultation use varied widely, with a 3.5-fold difference between the lowest and highest quartiles of use (p<0.01). In multivariate regression, patients ≥76-years-old received 0.3 fewer consults compared to those ≤49 years old (p<0.01). Uninsured and Medicaid patients received 0.2 fewer consults compared to Medicare patients (p<0.01). Hospitalist attending consultation use did not differ from non-hospitalists (p=NS). Patients cared for by hospitalists working with trainees received 0.1 fewer consults than those cared for by non-teaching hospitalists (p<0.01). Attendings likely to leave academic practice were associated with 0.3 more consults per admission (p=0.03). The number of consultations per admission decreased each year in the sample, with admissions in 2016 receiving 0.7 fewer than those in 2011 (p<0.01).
Conclusions: Significant variability exists in use of inpatient consultation. Understanding this variability may help identify patient and physician groups at high-risk for under or overuse of consultation and for subsequent development of interventions to improve high-value care.