Background: As hospital medicine looks to the future, we carry forward achievements and lessons learned from the past three years. In our large and diverse health system (with 14 acute care hospitals that serve adult inpatients from a populous catchment area, ranging in type from quaternary/academic to community based) we found we can best support our hospital teams with user-centric guidelines that incorporate updated evidence, internal expertise and scholarship, and available resources – and thus, maintain our commitment to delivering care at the highest standards, even in the face of a novel pathology. Leveraging this experience in deploying evolving recommendations for COVID-19, we established an infrastructure to design and disseminate care guidelines for high-yield, hospital-based, medical conditions across our system. These currently include guidelines for the inpatient management of bacterial pneumonia, decompensated heart failure, acute pain, and comfort care. The initiative’s overarching objective is to consistently deliver high-quality care with minimal, unnecessary variation to our hospitalized patients, equitably.
Purpose: Tailor evidence and expertise to design care guidelines and corollary EMR order sets that are practically useful at the point-of-care to all medicine providers (employed hospitalists, voluntary physicians, advanced care providers, residents) on primary and co-management services at our hospital sites.
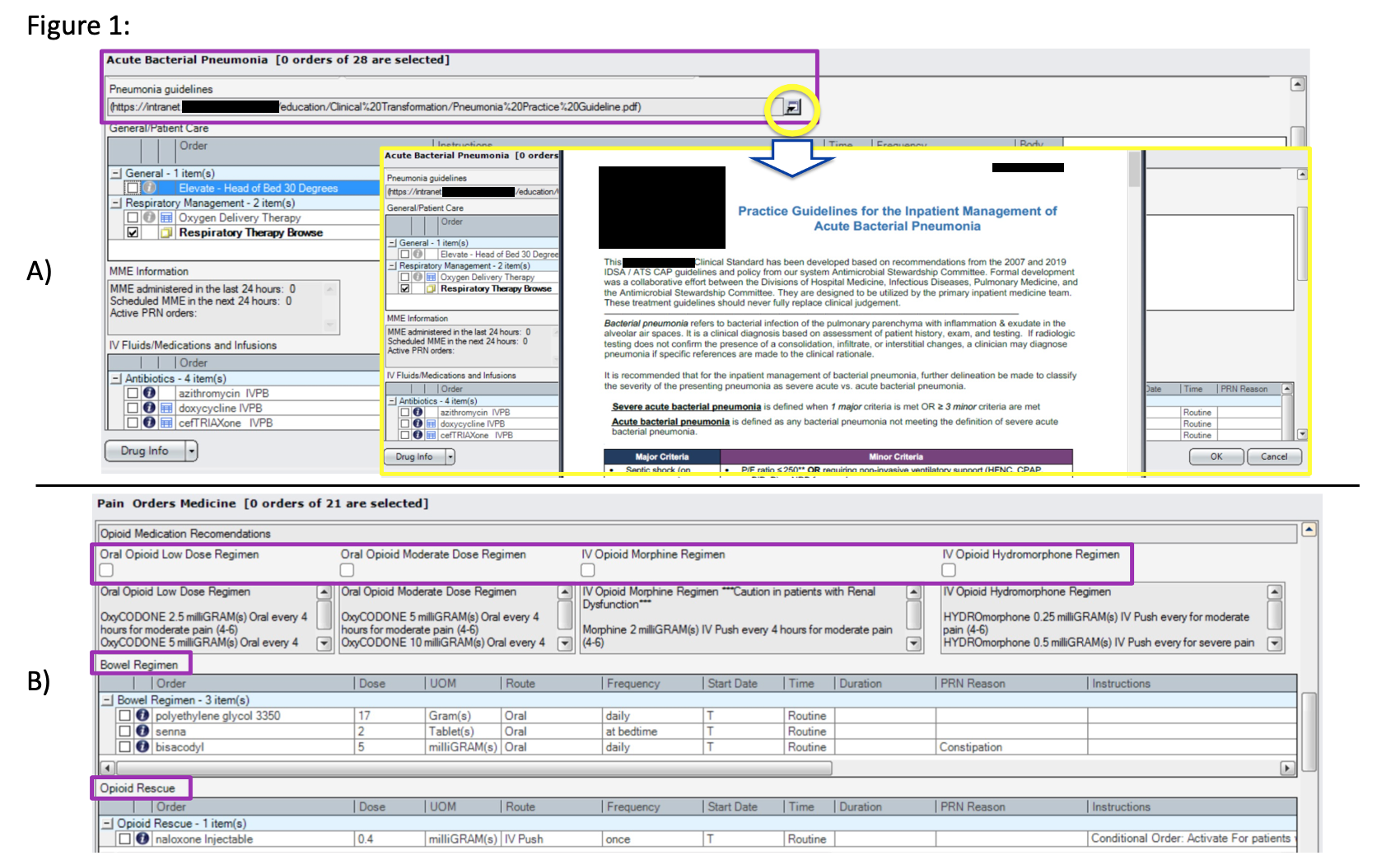
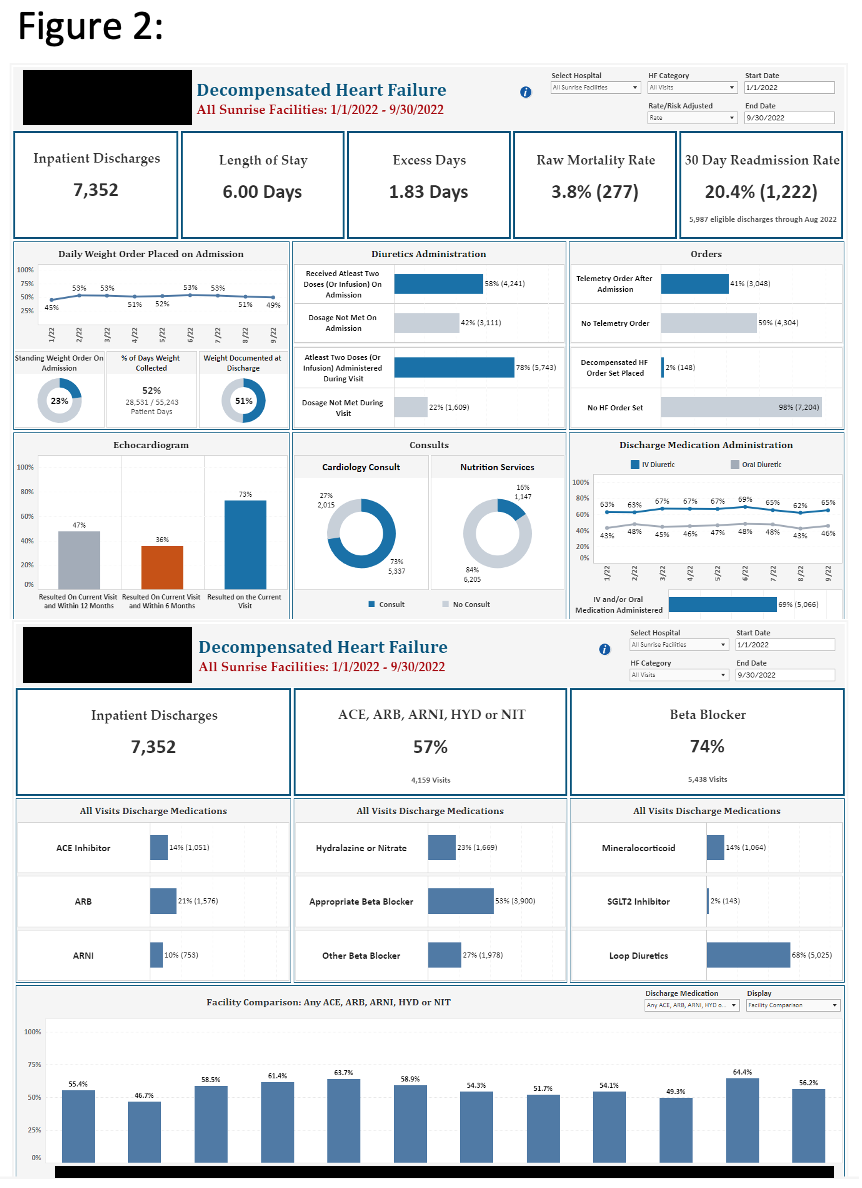
Description: There are four phases to the design and dissemination of each guideline: Convening, Content, Creation, and Circulation. Crucial to the design process is the convening of engaged stakeholders and subject-matter experts to review related data and updated society recommendations. Especially notable is ensuring those convened represent a diversity of perspectives of practicing in different inpatient settings with varying resources. During the content phase this group distills goals for each guideline, including discrete recommendations that match our context and communities, limit unintended consequences, and answer specific clinical conundrums. Priorities for monitoring and evaluation are also identified. Early engagement of leadership is valuable to ensure connection with kindred department, hospital, or system initiatives. The design process culminates with the creation of four products for each condition: a documented consensus care guideline and user-centric order set integrated into our enterprise EMR (Fig 1, A / B), an education plan to disseminate both to all appropriate audiences, and an interactive dashboard monitoring outcome and process metrics serving the priorities of clinicians, patients, administrators, and quality teams (Fig 2). The creation phase requires close partnership with EMR and data management teams. Critically, the circulation phase involves a multi-pronged approach of dissemination to ensure broad awareness and adoption, with the emphasis that each guideline should never fully replace clinical judgment.
Conclusions: The adoption of inpatient care guidelines enables the foundation of equitable care for our hospitalized patients upon which personalized care for each individual can be built. Further, with continued monitoring, evaluation, and amendment of each guideline as necessary per feedback, adherence metrics, and data evolution, hospital-based medical teams can be assured they are supported with curated, evidence-based, best practices to enhance the quality and efficiency of their care.