Background: In 2014 we recognized that the pace of admissions frequently exceeded our ability to assign a hospitalist. Long patient wait times occurred at admission, especially for patients arriving in the late afternoon when hospitalist day shifts were ending.
Purpose: To redesign hospitalist schedules, duties, and method of distributing admissions to match demand.
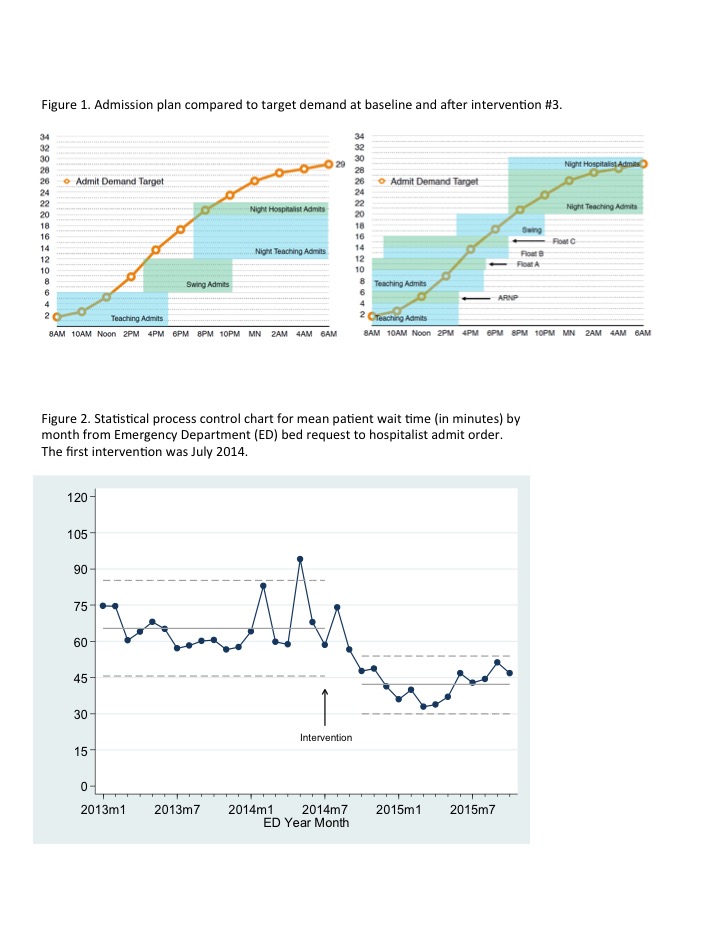
Description: We used administrative data to tabulate Hospital Medicine admission requests by time of day. We identified a mismatch between volume and capacity with the current staffing model. We learned our team needed to accommodate 29 admits per 24 hour day with peak admission volume in the late afternoon and early evening. The current staffing model failed after 22 admits when running smoothly (Fig 1).
To realign staffing around patient admissions, we organized a series of Lean quality improvements, starting with a 2 day Kaizen improvement event in July 2014, followed by a series of PDSA (Plan-Do-Study-Act) cycles. The improvement team included hospitalists, residents and administrators, and each PDSA cycle involved ample collection of feedback from all affected providers. We confirmed success with follow-up data on patient wait times, hospitalist satisfaction and cost.
INTERVENTION
Baseline: Our hospitalist group had 6 daytime and 2 nighttime services, including teaching services and attending-only services (swing and float). Four of 8 services were available for admissions while 4 were rounding-only. Admitting capacity (patients per day) was 22.
PDSA cycle 1: Our 4 teaching teams moved from every other day to daily admitting. A standard admit sequence was developed so each team rotated through admissions. Six of 8 services were available for admissions. Admitting capacity increased to 24.
PDSA cycle 2: We replaced the admitting only swing service with a float service with a later shift start time. An ARNP service was added. All 9 services were available for admissions with the daytime services sharing rounding and admitting work. Admitting capacity increased to 25.
PDSA cycle 3: The swing service was reintroduced to accommodate increasing admit volume. A second float service was changed to a later start time. All 10 services are available for admissions. Admitting capacity increased to 30 (Fig 1). FTE increased by 1 ARNP and 1 MD over the study period.
The final staffing model aligned with patient admissions (Fig 1). Emergency Department patient wait times for admission decreased 36% from 65.4 to 42.1 minutes (p<.001, Fig 2). Hospitalist professional cost per discharge decreased by 36%. Hospitalist “bad” days per month improved from 30% to 22%. Patient satisfaction and average length of stay were unchanged.
Conclusions: Quantifying admission demand by time of day, then designing work schedules and duties around meeting this demand can be an effective approach to reduce wait times and cost, and improve the experience of practicing hospital medicine.