Background:
Avoiding repeated complete blood count (CBC) tests in the face of clinical and lab stability is a focus of the Choosing Wisely initiatives endorsed by the Society of Hospital Medicine. The goal of this study was to identify situations in which routine CBC testing can be avoided.
Methods:
This was a retrospective study of 50 patients with community-acquired pneumonia (CAP) discharged from our hospital between 2/1/2015 and 5/1/2015. We performed chart abstractions collecting daily vital signs, lab results, assessment and plan, and orders, as well as documentation which indicated whether a lab result or clinical finding appeared to affect clinical management (e.g. a new order or documentation of changing plans). Vital signs were used to define clinical stability based on Pneumonia Patient Outcomes Research Team (PORT) study criteria. We used descriptive statistics and likelihood ratios to characterize the utility of CBC testing for producing clinical management changes.
Results:
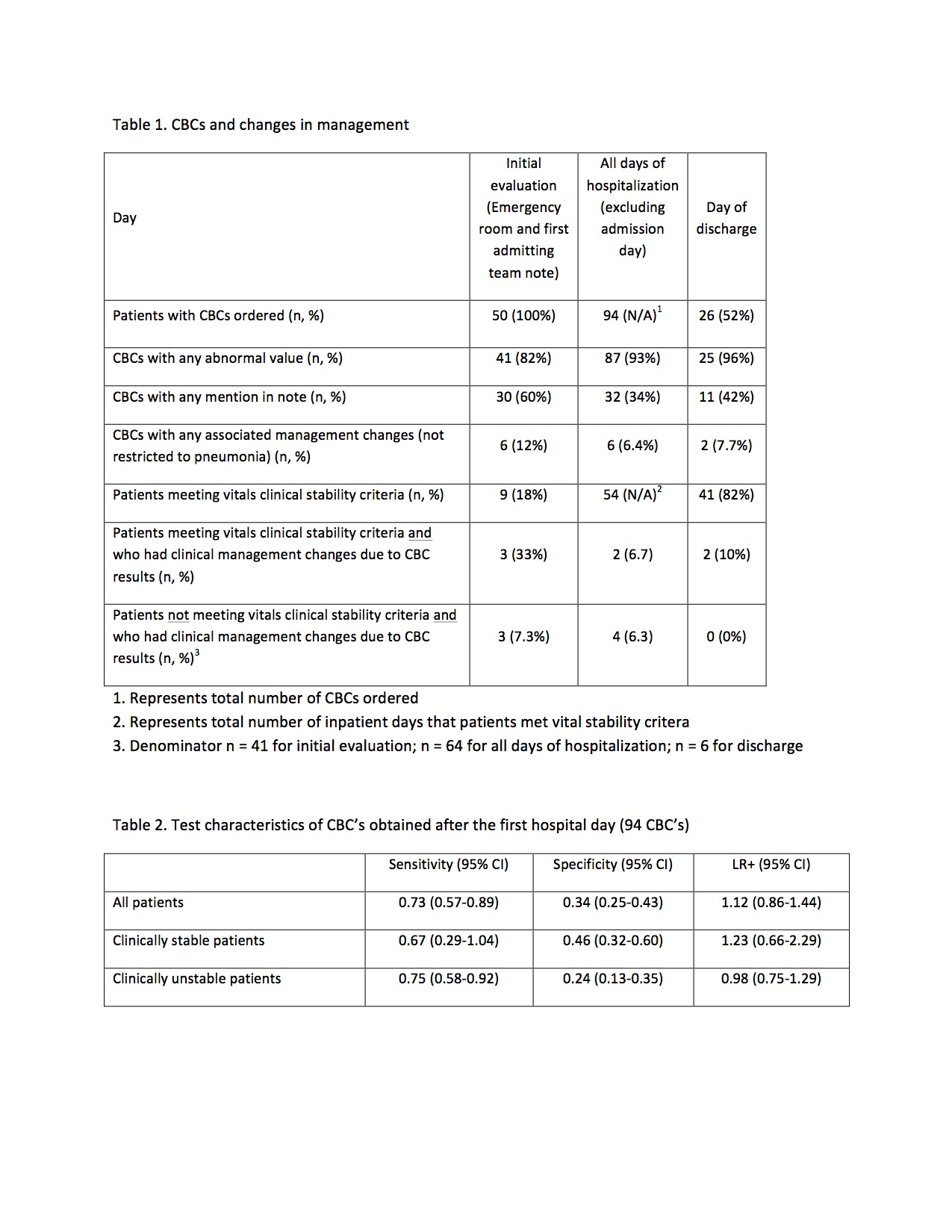
Of 50 patients, 33 (66%) were female, mean age was 75 years, mean length of stay was 2.8 days and median CURB-65 score was 1. On days after admission, 94 subsequent CBC’s were obtained. Of subsequent day CBCs, only 6 (5%) were associated with management changes indicated in documentation or orders. In all instances, additional diagnostic workup was obtained and CBC values improved without intervention. On the day of discharge (Table 1), 26 CBCs were ordered but no actions delaying discharge were taken and in only 2 of these cases was a lab value associated with a change in management (lab recheck and prescription for oral supplemental iron), and each was discharged that same day. The positive likelihood ratio of CBCs obtained after admission in terms of predicting a change in clinical management was 1.12 (95% CI 0.86-1.44) representing a 1.2% increase in the likelihood of a change in management based on the result. The positive likelihood ratio among clinically stable patients was still quite weak and with far wider confidence intervals (1.23, 95% CI 0.66-2.29) (Table 2).
Conclusions:
The likelihood of a CBC value changing clinical management among patients with CAP is low. CBCs obtained in stable patients by PORT criteria and on the day of discharge are unlikely to result in clinically meaningful changes in management.