Background: Critical event management skills are required for resident training. Critical events include rapid response events, acute clinical decompensation, and code blue events. Evidence supports simulation-based training to improve mastery and retention of these skills. We recognized a need for resident training in critical event management following concerns raised by interprofessional teams and safety event reports in our institution. In parallel to institutional efforts to standardize a script for the VA rapid response team, we developed a simulation-based emergency response curriculum for residents.
Purpose: Critical event management is a fundamental set of skills for internal medicine residents. In response to safety concerns reported at our Veterans Affairs hospital, we developed a simulation-based emergency response curriculum for PGY2 internal medicine residents. This curriculum also fulfilled a program goal of increasing participants’ knowledge, skills, and attitudes on responding to patient emergencies with graduated autonomy. This will hopefully translate into reducing patient safety events at our institution.
Description: Residency program leaders and attending physicians identified goal knowledge, skills, and attitudes for resident performance in critical event management. We designed a one-hour interactive didactic session addressing these competencies and teaching the new institutional standardized rapid response framework. Learners then practiced these competencies through six patient scenarios over two sessions in the VA Simulation Center. We assessed the impact of the education innovation on knowledge and on self-assessed preparation and attitudes regarding critical event management. Participants completed a knowledge assessment and attitudes questionnaire before and after the didactic session and simulation. Analysis was performed via Chi square testing on the data from initial and final responses of unmatched residents.
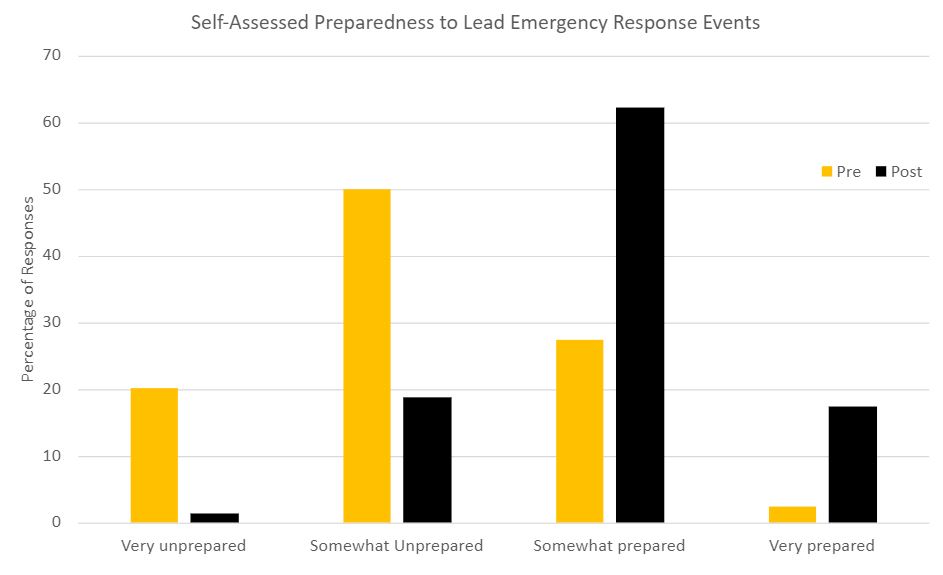
Conclusions: Pre-survey data showed that most respondents (70%) felt unprepared to lead patient emergencies supervised by a more senior physician (attending or fellow). This was expected as many interns have limited experience in this arena. After the training experience, most residents (79.6%) reported feeling prepared to lead a patient emergency while supervised (p< 0.01). Figure 1 presents the learners’ self-assessed feelings of preparedness for supervised leadership of emergency response events. Correct responses to knowledge-based questions were significantly (p< 0.05) higher for recall of dose and administration of epinephrine (76% to 94% correct) and when to use defibrillation (85% to 94% correct). Simulation based training led to immediate retention of knowledge and improved perceived preparedness in critical event management. This curriculum was effective at aligning medicine residents’ knowledge, skills, and attitudes with the institutional safety culture. This work also highlights the importance of involving education leaders in patient safety reporting data and trends. Awareness of those trends empowers educators to design curricula to target specific gaps and ideally improve patient outcomes.