Background: Cross-covering patients overnight is part of standard Hospitalist practice, however there is little understanding of the workload contribution. Much of the current literature for hospitalist productivity focuses on wRVU, day census, or number of admits per shift. These metrics are not applicable to cross cover since it is largely non-billable work. A cross sectional, web-based national survey study demonstrated hospitalist providers were less likely to agree they could provide safe care if they had more than 5 admissions per night (Atlas et al, 2021). Currently there is no standard to objectively measure workload for night shifts. The objective of this study is to determine the time cross cover contributes to nocturnist workload.
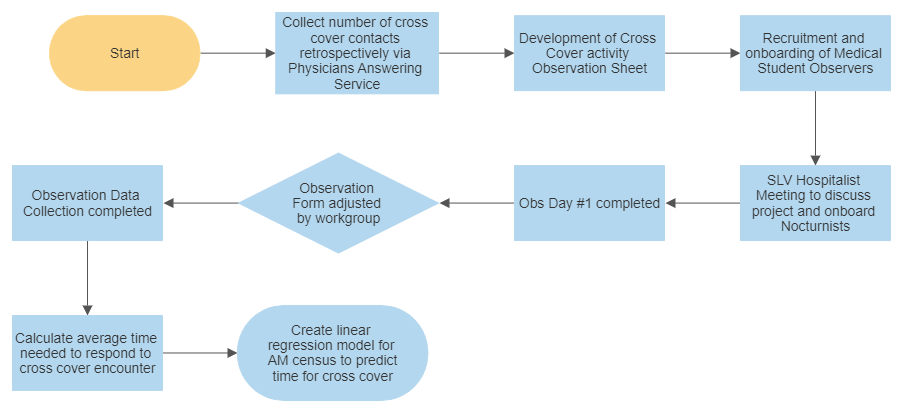
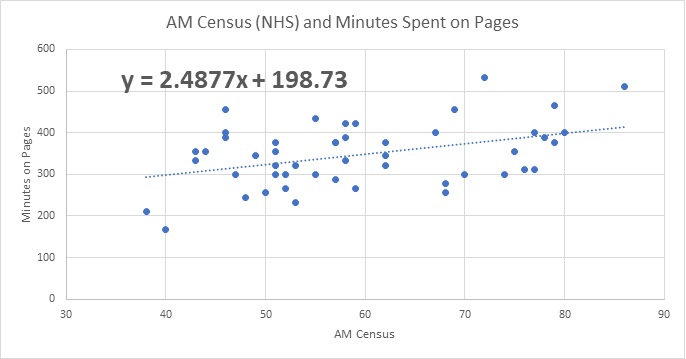
Methods: Our Salt Lake Valley Hospitalist service at Intermountain Medical Center (IMC) was chosen as a pilot site for several reasons: patients are Med-Surg status at a complex quaternary care center, total team patient census is high, and the primary mode of communication from outside callers to hospitalist is via one communication modality with reliable record of page counts (Physicians Answering Service). The project was phased, with initial review of all transcribed Physician Answering Service pages on 48 randomly chosen dates between March 2021 to March 2022 during the hours of 6 PM – 6 AM. Pages requesting admission or consultation were excluded. Next, a medical student volunteer directly observed nocturnists work for eight 6-hr shifts during which they timed every cross-cover encounter with a stopwatch. Along with the duration of each cross-cover encounter, additional data was collected: if a bedside visit was required, orders placed in the EMR, documentation was placed in the EMR, or if any interruptions to a current admission or interruptions to another cross-cover encounter occurred. Using these data elements, we created a linear regression model based on AM census to predict total cross-cover workload in terms of time. (Figure 1)
Results: The average number of pages per night shift was 32.2. With our medical student direct observation data, we found the time required to complete a cross-cover encounter was highly variable with a max of 185 minutes and a minimum of 1 minute. The average time per cross-cover encounter was 11 minutes. Based on our observational data and using our operations census dashboard, a linear regression equation was created as an estimation tool for cross-cover time: y = 2.4877x + 198.73 (x= total AM census and y= total minutes for cross cover). (Figure 2)
Conclusions: The estimation tool was created with the aim of understanding cross cover as a necessary component of nocturnist work. We have demonstrated that cross-cover is a quantifiable workload. This important clinical work should be taken into consideration when determining appropriate staffing needs. For example, using the tool, we can estimate the total cross cover minutes per night shift at IMC for an AM census of 111 would equal 7.9 hours. Annualized, this would represent 2,885 hours, which is equivalent to 1.4 FTE. It is critical that we continue work to fully assess hospitalist workload, productivity, and value. This work will allow hospitalist team models to evolve with the goal to provide high quality, safe, cost-effective options to address non-billable work, in addition to overall nocturnist workload.