Background: Both inappropriate hospital admissions and inappropriate discharges from the ED are associated with adverse patient outcomes. Little is known about the accuracy (sensitivity and specificity) of the hospital admission triage process.
Purpose: We sought to understand the operating characteristics of our triage process to identify opportunities for improvement and project an optimal model.
Description: Data was extracted from the electronic health record (EHR) of a 900-bed urban academic safety net hospital, covering a period of 4 weeks starting September 15, 2017 for all patients admitted to a non-ICU medicine service.
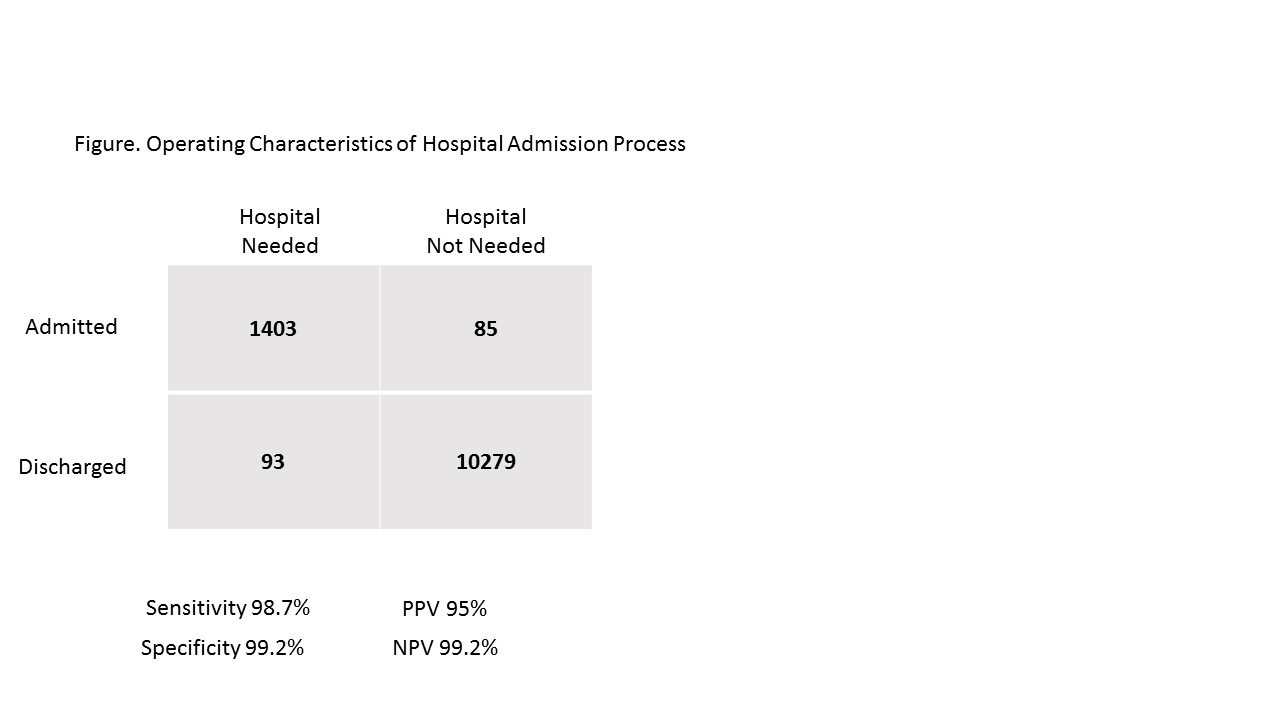
Patients discharged home within 24 hours of admission were identified as potential inappropriate/false positive admissions. Potential false negative/inappropriate discharges from the ED included all patients discharged from the ED who returned and were admitted to a non-ICU medicine service within 72 hours. True positives were identified as patients admitted for more than 24 hours. True negative discharges from the ED were not admitted within 72 hours of discharge.
Potential false positives and false negatives were reviewed by a panel including board certified internal medicine and emergency medicine physicians. After review, patients who did not require hospital admission were deemed actual false positive admissions and patients who met admission criteria on first ED visit were deemed actual false negative discharges from the ED.
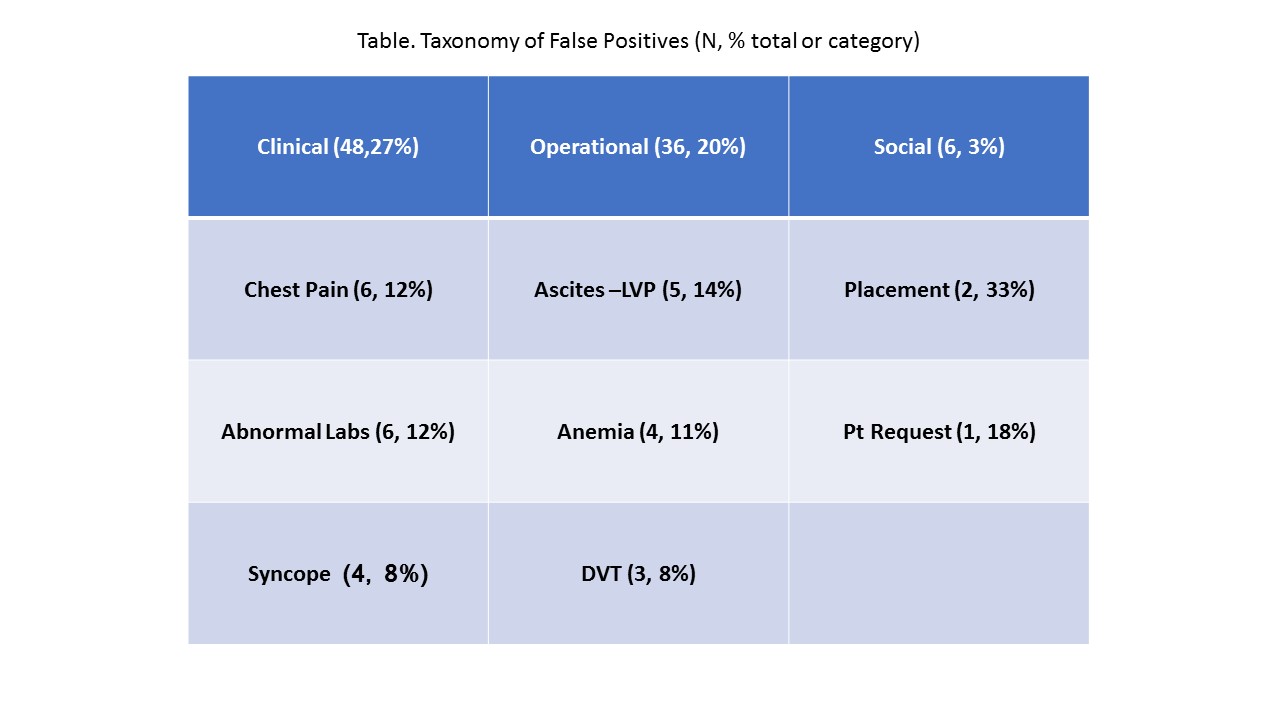
Actual false positive admissions were further categorized into clinical, operational, and social factors.
Conclusions: 1,488 of the 11,860 patients (12.5%) seen in the ED evaluated in the 4 weeks were deemed to need hospital admission. See Figure for sensitivity, specificity, positive and negative predictive values. See Table for clinical, operational, and social reasons for unnecessary admissions.
While sensitivity and specificity are both high, contrary to popular perception, our admission triage process results in a higher specificity than sensitivity. Of the 53.1 patients/day admitted, we identify 3.0 patients/day as false positives. Our greatest opportunities lie in clinical and operational improvements. By decreasing our unnecessary chest pain, large volume paracentesis and admissions for isolated lab abnormalities by 50%, we hope to achieve a specificity of 99.5% within 6 months without affecting sensitivity. False positives due to social issues may not reflect actual rates due to LOS over 24 hours. Real time monitoring and feedback could be utilized to maintain operational efficiency. Collaboration with other health systems can result in a consensus model for hospital admission triage operations.