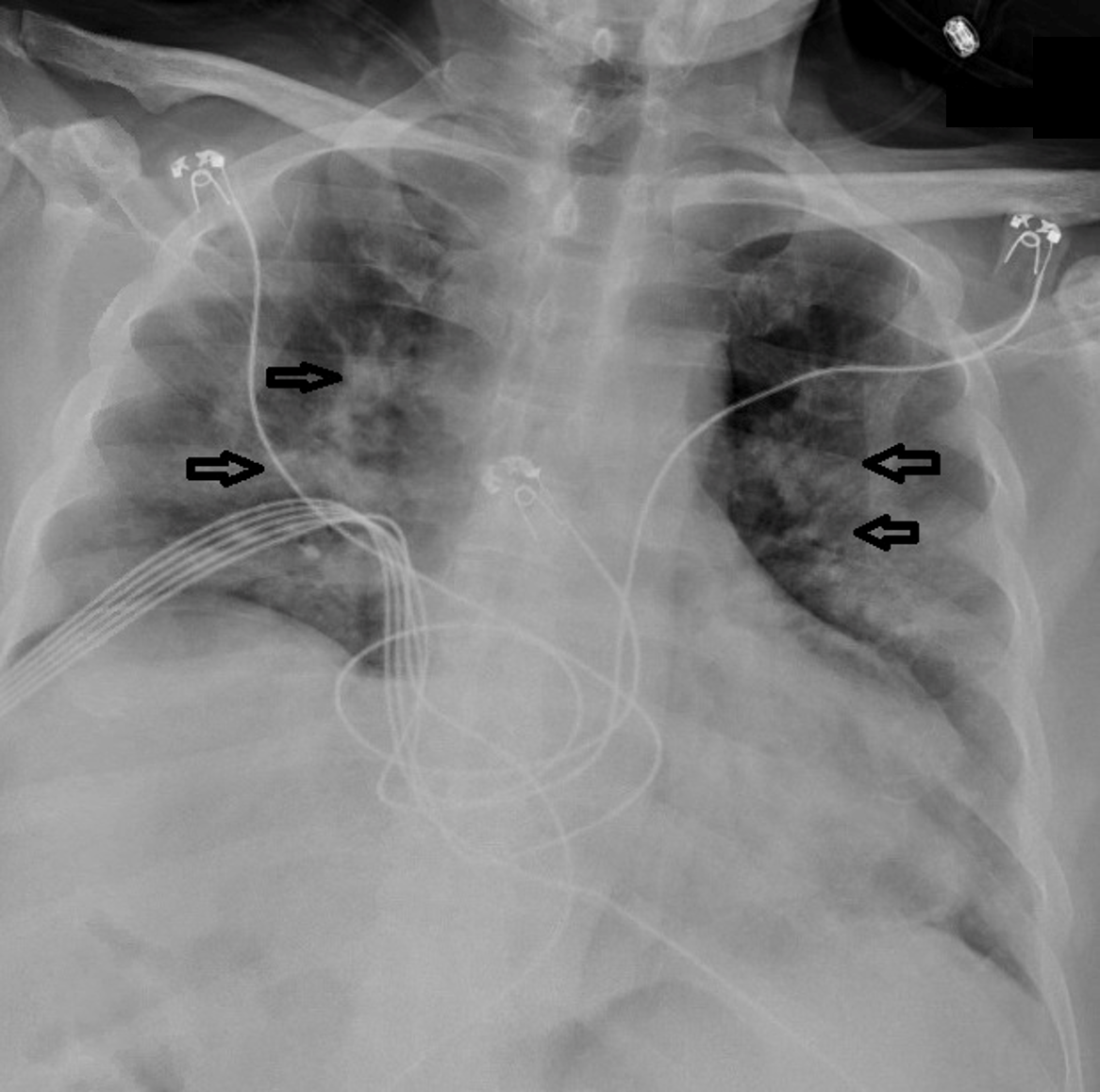
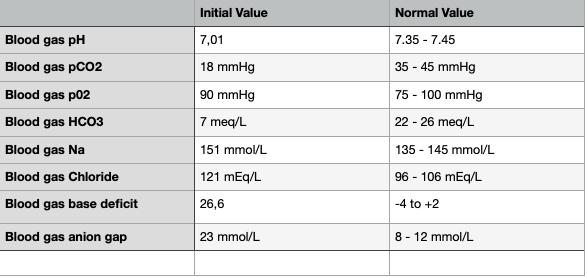
Case Presentation: A 52-year-old Hispanic man with a medical history of hypertension, T2D with neuropathy, and hyperlipidemia without previous exposure to glucocorticoid presented to the emergency department (ED) with mild fever, headache, and shortness lasting three days. His diabetes had been well controlled with glipizide, metformin, and liraglutide, and his recent glycated hemoglobin was 7.2% (two months before presentation). His initial blood glucose level was 415 mg/dL with positive serum ketone of 5.8 mmol/L (reference range: 0.0-0.27 mmol/L) and urine ketone was 40 mg/dL (reference range: <0 mg/dL). His initial arterial blood gas investigation was shown in the table 1. Complete blood count showed elevated white blood cell counts of 23,100/µl (left shift neutrophil leukocytosis of 18,711/µl and neutrophil-to-lymphocyte ratio [NLR] of 13.5). D-dimer assay revealed 4,031 ng/mL (reference <318 ng/mL). Inflammatory markers showed raised wide range C-reactive protein (CRP) levels at 14.122 mg/dL and increased ferritin at 1434.4 ng/mL (reference range: 3.1-110.9 ng/mL). Chest x-ray revealed bilateral pulmonary infiltrates compatible with COVID-19 pneumonitis (Figure 1), and the diagnosis was confirmed with a positive SARS-CoV-2 ribonucleic acid PCR test. We tested his serum C peptide level on the second day of his admission to assess his endogenous insulin secretion status, and it was low (0.6 ng/mL; reference range: 1.1-4.4 ng/mL) with a blood glucose of 193 mg/dL indicating the patient was in an insulinopenic state while his serum lipase level was in the reference range. He was admitted to the ICU and treated with intravenous (IV) fluid and rapid-acting insulin infusion with closed monitoring of arterial blood gas for AG and serum sodium, chloride, bicarbonate, potassium magnesium, and phosphate every four hours. Every hour, we assessed his blood glucose levels and respiratory status for DKA, and we checked for respiratory distress. He was given IV ceftriaxone 500 mg, twice daily, oral hydroxychloroquine 200 mg once daily, and oral azithromycin 250 mg once daily, with supportive care. His DKA resolved after 39 hours of insulin infusion with closed AG. On the 21st day of hospital admission, he was discharged with the continuation of the same regimen of oral home anti-hyperglycemic medications.
Discussion: The transient damage of pancreatic beta-cell function leading to reduced levels of serum C peptide may be the reason for our patient experiencing acute insulin-dependent DKA for a brief period during the course of COVID-19. In the respiratory system, ACE2 is necessary to break down angiotensin II to angiotensin 1-7, which are involved in the Mas receptor pathway to counteract inflammation and fibrosis. Therefore, a SARS-CoV-2 infection with the deployment of ACE2 yields a decline in the body’s defense mechanism alongside imbalanced metabolic function, leading to DKA and multiorgan dysfunction [1], [2].
Conclusions: COVID-19 patients with T2D may present with unusual presentations of DKA. COVID-19 may cause DKA by increasing insulin requirement induced by ACE2-mediated destruction of pancreatic beta cells, as evidenced by reversible decreased serum C peptide levels or other unexplored mechanisms. Physicians should be aware of COVID-19 with a concomitant increase in the risk of DKA patients with T2D. However, more studies are needed for a better understanding of the pathogenesis of DKA in patients with coexisting T2D and COVID-19, and the prevention of poor outcomes in patients with diabetes.