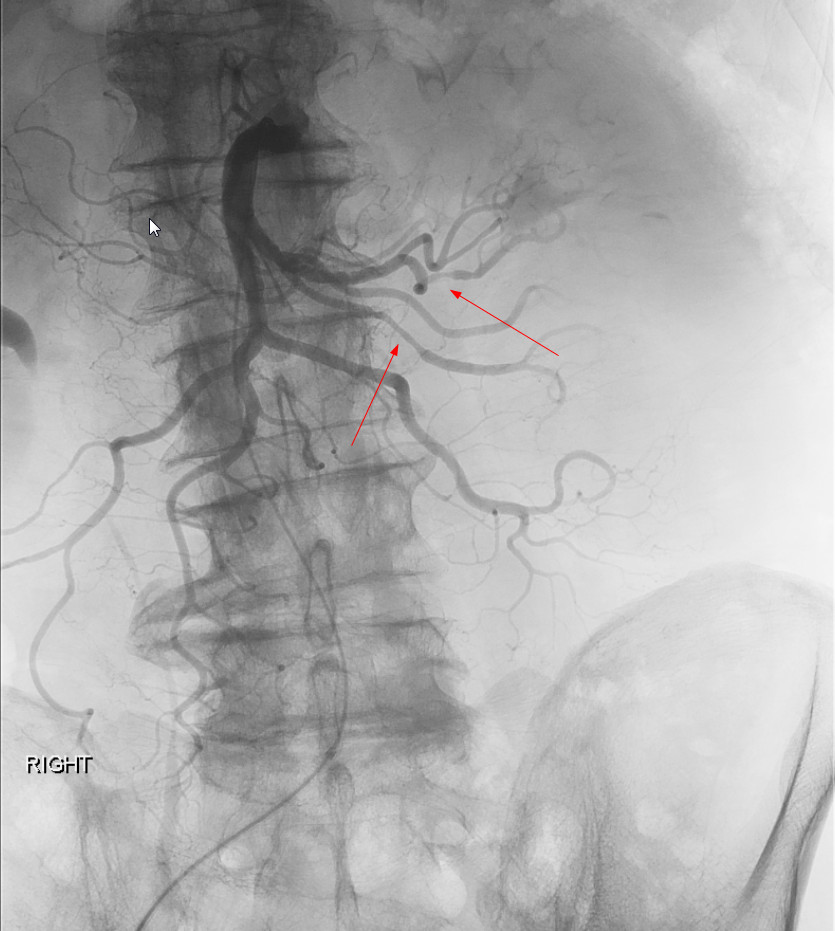
Case Presentation: 76-year-old male with a recent diagnosis of low-grade MDS presented to the hospital with complaints of severe fatigue, anorexia, abdominal pain and a 60 pound weight loss over six months. He also had a history of right foot drop 2 months prior with unclear etiology. He was subsequently hospitalized 1 month before presenting to our hospital with increasing abdominal pain, CT abdomen showed ileitis and mesenteric lymphadenopathy. He was treated with broad spectrum antibiotics with minimal improvement. Initial studies at our hospital showed pancytopenia with values near baseline, an elevated sedimentation rate of 82 mm/hr and C-reactive protein of 72.5. He had normal electrolytes, creatinine, copper, vitamin B 12 and vitamin-D levels. Urinalysis was within normal limits and serum protein electrophoresis did not show any monoclonal proteins. Complement and cryoglobulin levels were within normal limits. His serologies including ANA, ANCA, antiphospholipid antibody levels, hepatitis B and C were within normal limits. EMG of the lower extremities showed involvement of right distal sciatic nerve or both tibial and peroneal nerves. Colonoscopy revealed nonspecific inflammation of the colon. CT angiography revealed aortoiliac atherosclerosis but no evidence of vasculitis. Mesenteric angiogram was ordered due to high suspicion for vasculitis which revealed areas of narrowing along the superior & inferior mesenteric artery. This confirmed a diagnosis of polyarteritis nodosa (PAN). Following this the patient was given pulse dose steroids for 2 days followed by a slow taper. Further evaluation of MDS with T-cell receptor analysis was recommended.
Discussion: Hospital admissions for chronic medical conditions often pose management difficulties for hospital services. This case highlights that clinicians admitting patients with worsening of systemic symptoms of unclear etiology with previous hospitalizations should broaden their differential to include vasculitides. PAN is a necrotizing medium vessel vasculitis affecting vascular supply to critical organ and may rarely be associated with MDS. Early diagnosis and facilitation of testing in the hospitalized setting are critical for decreasing complications in cases of vasculitis.
Conclusions: PAN should be considered in patients with a constitutional symptoms and signs of organ involvement such as abdominal pain or mononeuritis multiplex. In patients with MDS, symptoms concerning for PAN should prompt evaluation for vasculitis. Treatment is based on severity. Involvement of the gastrointestinal or cardiac system should warrant treatment with prednisone and immunosuppressive therapy. In cases where PAN is associated with MDS, alternative options have to be considered.