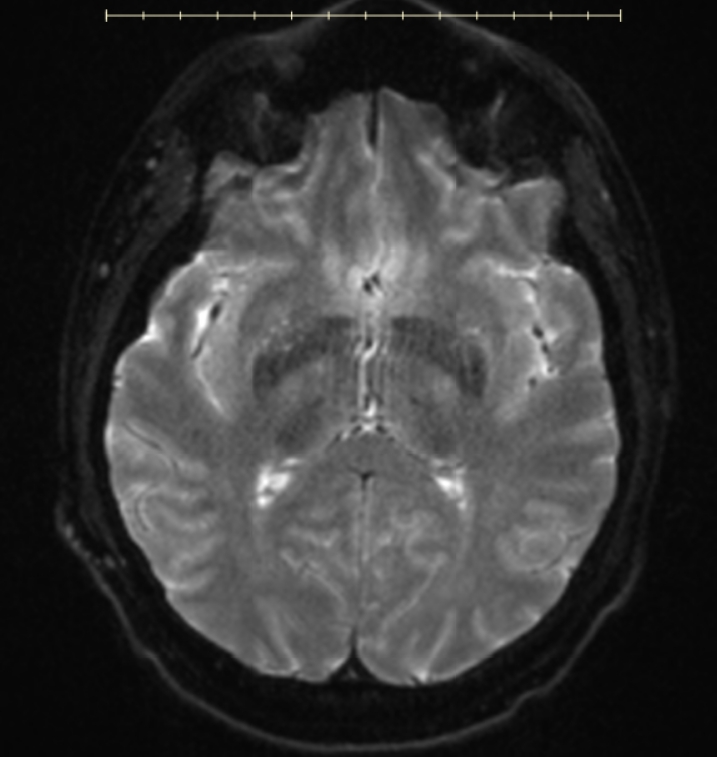
Case Presentation: A 33-year-old man sought medical evaluation due to an ongoing cough which had persisted following infection with COVID-19. His chest xray (CXR) was negative at that time and he was discharged with symptomatic treatment. He presented again five months later due to persistent cough non-responsive to symptomatic treatment and underwent another CXR which revealed patchy airspace disease concerning potential pneumonia. His cough slightly improved with antibiotic therapy, however, follow up CXR continued to show worsening patchy opacity in the right upper lung suspicious for pneumonitis. CT thorax with contrast was performed and revealed right upper lobe mass-like opacity with tethering of the subpleural lung and enlarged mediastinal and right hilar nodes. Transbronchial biopsy showed organizing pneumonia with atypical cells on bronchoalveolar lavage concerning for a reactive process. He was treated with corticosteroids for organizing pneumonia with partial improvement in symptoms. A PET scan demonstrated the progression of right lung mass and left pleural lesion along with destruction of ribs 1-2. Given the patient’s young age and lack of risk factors for lung cancer, consolidated pneumonia or infectious etiology was favored. He was admitted to the hospital for a repeat lung biopsy which revealed necrosis and fibrosis. An extensive infectious workup, including universal PCR, was negative. MRI of brain was performed to rule out nocardia or distant infectious metastasis causing brain abscess. The patient was found to have multiple ring-enhancing lesions throughout bilateral cerebral parenchyma and left cerebellum. Due to inconclusive results of prior biopsies and concern for a progressive process, brain biopsy was performed and revealed discohesive atypical cells with rhabdoid morphology with loss of INI-1 nuclear staining consistent with INI-1 deficient tumors of the mediastinum/lung or epithelioid sarcoma.
Discussion: SMARCB1/INI1 gene is one of the tumor suppressor genes and loss of function mutations lead to aggressive rhabdoid tumors. Being a diverse group of tumors with mixed phenotype, they often contribute to a diagnostic conundrum.SMARCB1/INI1 gene deficient tumors are extremely rare and present most commonly in young men. The difficulty in diagnosis in this case was attributed to the rapid tumor growth which outstripped its blood supply, leaving behind necrotic tissue. This is why repeated pathology specimens showed only necrosis or abnormal inflammatory tissue which was read as consistent with pneumonitis or pneumonia or atypical cells which were too necrotic to characterize. We were lucky that the larger, leptomeningeal arteries were included in the brain biopsy, which revealed live tumor cells ringing these vessels, surrounded by further necrotic tissue. The parenchymal vessels tend to be small and were unable to support tumor survival, leading to negative biopsies.
Conclusions: This case helps to highlight the consideration of SMARCB1/INI1 deficient tumors in cases of refractory pneumonia and reinforces the need for ongoing imaging follow up even in young patients with cough whose symptoms do not resolve. Additionally, in patients with atypical infectious findings, such as adjacent bone involvement and growth despite appropriate therapy, atypical malignancies must remain on the differential.