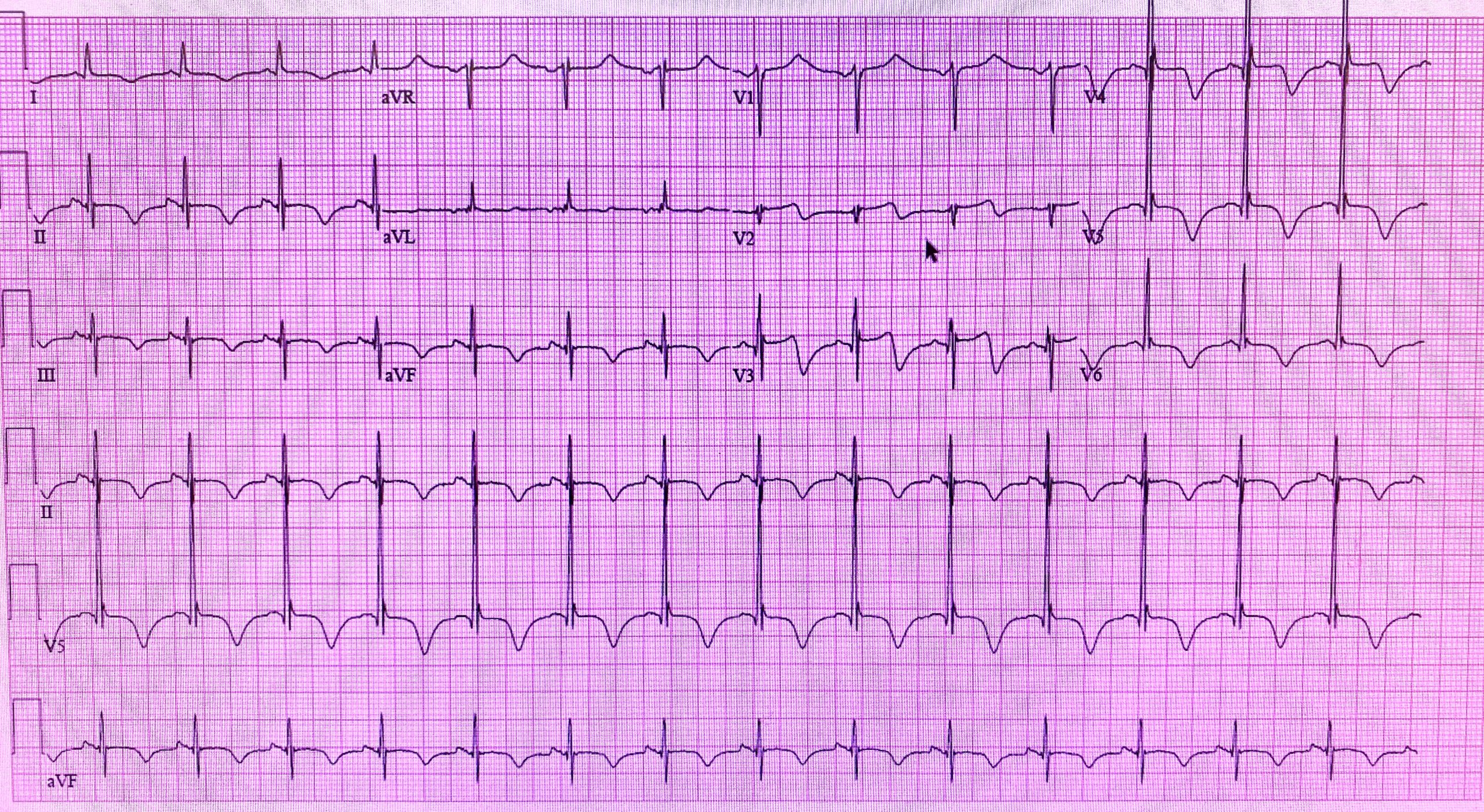
Case Presentation: Patient is a 61-year-old male found lying only partially clothed in a church courtyard brought in by EMS, hypothermic on arrival and tachycardic in the 130s. HRs improved with hydration and warming. Patient became verbally aggressive and threw himself on the floor multiple times. Initial troponin noted to be 4 peaking at 6.2. His drug screen was negative. His other labs were within limits with the exception of a low pre albumin and high BUN improving with fluids. EKG demonstrated prolonged QT intervals with diffuse deep T-wave inversions throughout. He was treated initially with haloperidol before the first EKG. A CT scan was obtained as there was concern for cerebral hemorrhage given the patients altered mental status as well as concern for “cerebral” T waves. CT returned negative for acute pathology and he was then started on heparin, aspirin and medicated with olanzapine. Echocardiogram notable for nondilated left ventricle with hypokinetic mid and distal anterior wall, mid anteroseptum and apical lateral wall and moderately decreased systolic function with ejection fraction of 35-40%. Cardiology determined it was best not to pursue an ischemic workup at this time as the patient’s potential compliance for antiplatelet therapy required for a stent placement was a major concern. It was felt that the EKG changes and troponin are consistent with NSTEMI, probably related to demand ischemia from hypothermia, tachycardia, and hypovolemia.
Discussion: The differential for deep T wave inversions on electrocardiogram (EKG) can be broad and includes several different disorders such as myocardial ischemia, pulmonary embolism, ventricular hypertrophy, and increased intracranial pressure. The finding is quite rare and the underlying mechanism is unknown. It is hypothesized that increased sympathetic tone due to central nervous system (CNS) insult is the cause. Uniquely in CNS insult, diffuse T wave inversions are seen rather than being limited to a single EKG territory. The recognition of cerebral T waves can have significant impact on a patient’s clinical outcomes. These findings along with a prolonged QT interval, Osborn (J) waves and U waves are associated with intracranial hemorrhage (ICH) and increased intracranial pressure. Unfamiliarity of this finding on EKG can lead to catastrophic outcomes in patients who go undiagnosed with intracranial hemorrhage. Many physicians associate T wave inversions with myocardial infarction or pulmonary embolus thus leading to preemptively initiating anticoagulation without recognizing that the patient’s etiology of symptoms may be due to CNS pathology.
Conclusions: The differential for deep T wave inversions on EKG is very broad. It is essential for physicians to consider a neurologic source for EKG alterations mentioned above prior to initiating heparin which may provide a theoretical mortality benefit.