Background:
Late discharges are a major problem across VCU Health Systems. Only 10% of pediatric patients are discharged before noon, and over 1/3 of patients are discharged after 5 PM. Late discharges delay admissions and transfers from ED, PICU, and outside facilities. Late discharges disrupt nursing and physician workflow, create additional burden during a time period when residents and nurses are admitting new patients, and create bottlenecks in the ED. With the discharge before noon (DBN) organizational goal of 30%, we describe a quality improvement initiative of a discharge huddle to improve our DBN rate.
Purpose:
A discharge huddle project team was created and consisted of medical director of inpatient services, director of quality improvement, nurse manager of acute care pediatrics, and the nurse educator. Daily discharge huddles took place at 3:30 pm Monday‐Friday. The discharge huddle project team along with unit charge nurse and senior residents from the two inpatient teams participated. All discharges that were targeted for the next day were identified. During the huddle, a ‘discharge checklist’ of items that needed to be completed if the patient is to be discharged in a timely fashion was reviewed. The checklist was maintained by the nurse manager. Using this checklist, we were able to identify recurring factors that interfered with early discharges and provide feedback to the senior residents the next day.
Description:
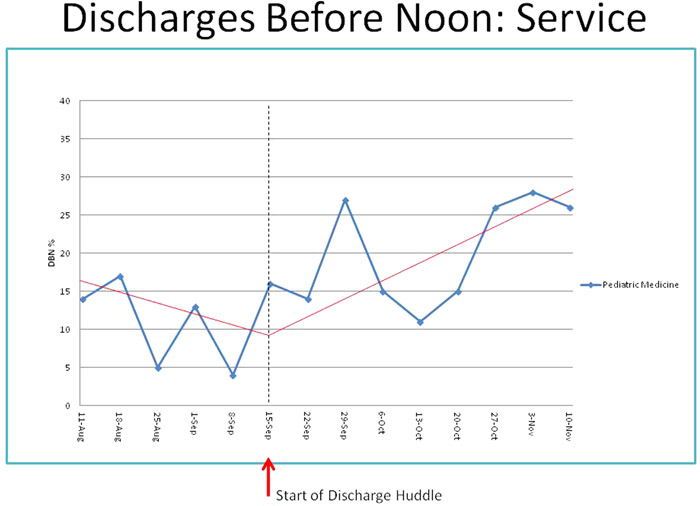
In the six weeks preceding the huddle, the average DBN rate was 11.5%. Since the initiation of the huddle, the average DBN rate improved to 20.3%. For pediatric hospitalists who serve as the inpatient teaching attending, the DBN rate improved from 12.7% to 18.6%. In terms of discharges after 5pm, there was a modest decrease from 35.1% prior to the huddle to 31.8% after the huddle. However, for the pediatric hospitalist patients, discharges after 5pm rate dropped from 34.8% to 27.5%. Recurring factors that delayed early discharges were: parents not aware of the discharge plan; nurses not aware of the discharge plan; discharge plan not fully discussed with the patient’s attending physician; and discharges delayed by pending procedures such as: pulmonary function tests, physical or occupational therapy evaluation, care coordination, and patient transfer arrangements with outside facilities. Residents and nurses reported improved collaboration and communication regarding the discharge process.
Conclusions:
Although we did not meet the organizational goal, we were able to increase DBN rates using a multidisciplinary approach and enhanced communication between different stakeholders. The huddle raised the consciousness to the importance of efficiency in the discharge process, gradually building it into the daily routine. The use of the checklist and next day feedback to residents have played a positive role in the overall communication and planning of effective and efficient discharge process.