Background: Patients with limited English proficiency (LEP) face barriers communicating with their medical providers and understanding their treatment plans. Prior work shows that communication barriers limit LEP patients’ understanding of their discharge instructions. However, little is known about disparities in outcomes between LEP and English proficient (EP) patients. To address this gap, we measured the prevalence of patient-reported, post-discharge outcomes among more than 18,000 LEP and EP patients.
Methods: We performed a retrospective cohort study at two hospitals at the University of California, San Francisco. Eligible patients were at least 18 years old and were discharged home from a medical or surgical service between May 2018 and April 2019. We obtained demographic, clinical, and discharge data from the electronic medical record. Within 72 hours of hospital discharge, patients received an automated phone call that asked about six post-discharge outcomes: discharge instruction questions, follow up care questions, new or worsening symptoms, medication concerns, needing help to get prescriptions, and questions regarding any other clinical issues not listed. Patients could answer in English, Cantonese, or Spanish. Trained care transitions nurses made follow-up calls to patients with reported issues and to patients who did not respond to automated calls. If patients stated their preferred language for care was not English and they needed an interpreter, we characterized them as LEP. We assessed differences in baseline characteristics using the chi-square and Wilcoxon rank sum tests. We determined the association of English proficiency and post discharge outcome using log-binomial generalized linear models adjusting for demographic differences and accounting for repeated observations.
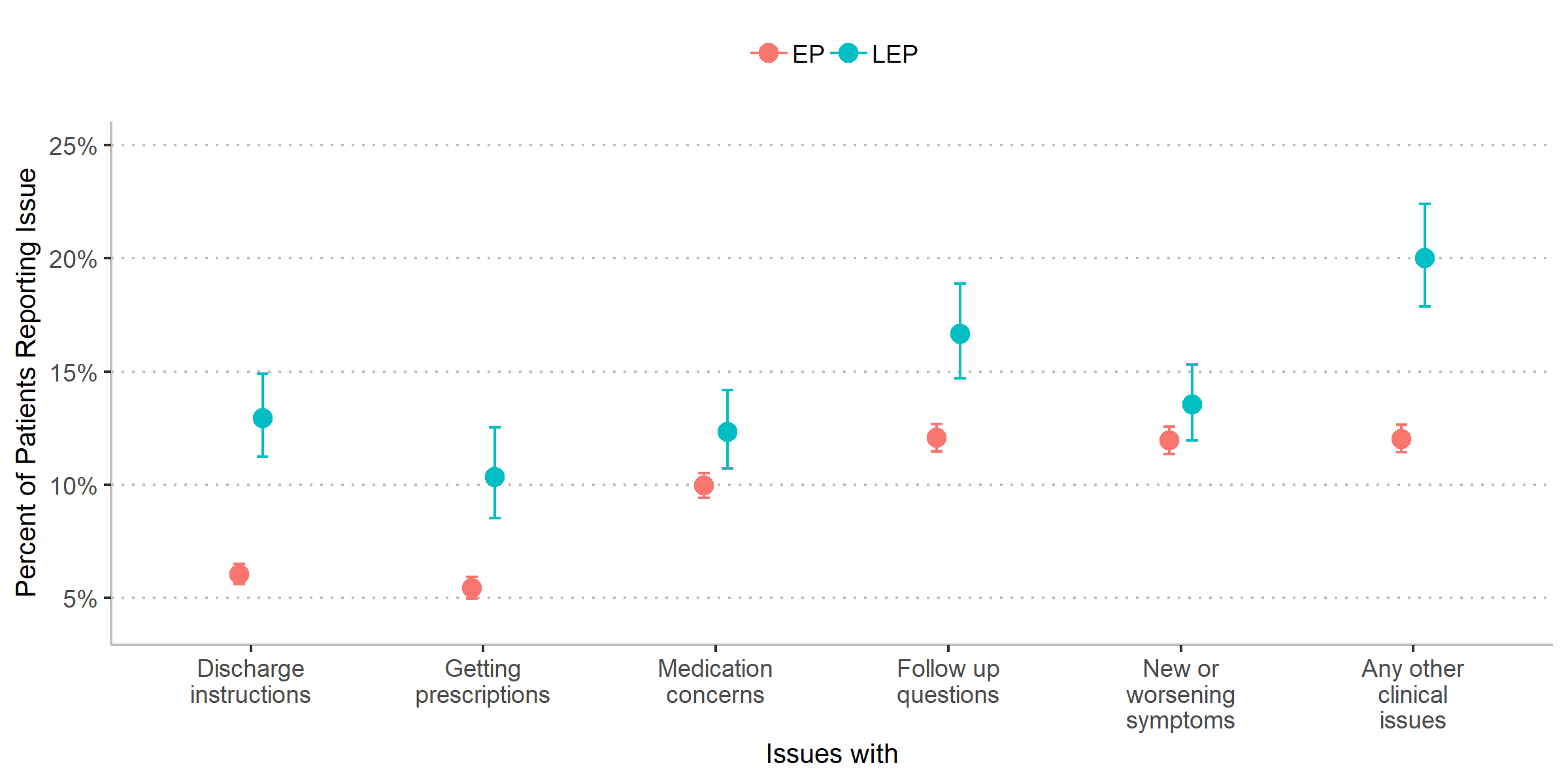
Results: Of the 18,463 eligible discharges, 79% responded to an automated or manual phone call, and 12% were LEP. The LEP patients were more likely to be older (median 65 years for LEP patients vs. 57 years for EP patients, p<0.001), insured through Medicaid (37% vs. 22%, p<0.001), and either Hispanic (41% vs. 14%, p<0.001) or Asian (44% vs. 12%, p<0.001). Compared to EP patients, LEP patients reported more post-discharge issues in 5 of the 6 domains assessed (Figure). LEP patients were more likely to report discharge instruction questions (13% vs. 6%, p<0.001), follow up care questions (17% vs. 12%, p<0.001), medication concerns (12% vs. 10%, p=0.005), needing help to get prescriptions (10% vs. 5%, p<0.001), and having other clinical questions (20% vs. 12%, p<0.001). LEP patients did not report significantly higher rates of new or worsening symptoms (14% vs. 12%, p=0.06).
Conclusions: Compared to EP patients, LEP patients face disparities in multiple domains after hospital discharge. These disparities may stem from the quality of inpatient care, discharge counseling, or access to care following discharge. Processes tailored to LEP patients need to be tested and implemented to mitigate observed disparities.