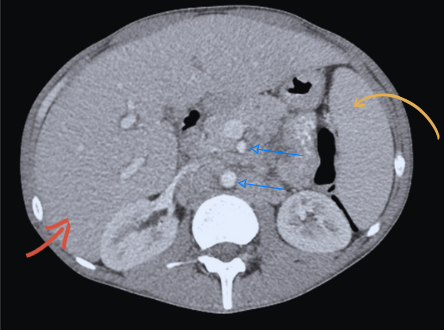
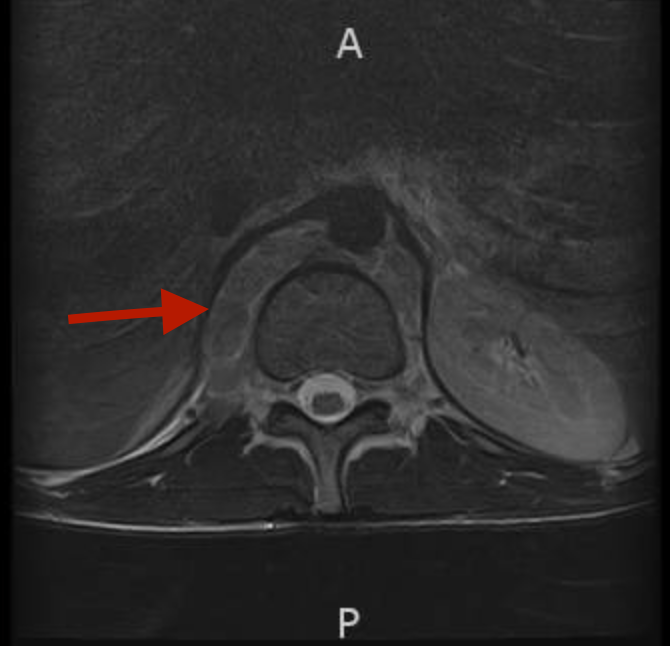
Case Presentation: A 27-year-old male with a past medical history of HIV, poorly adherent to antiretroviral therapy (ART), presented with a 1-month history of worsening lower back pain. Pain was described as 10/10 in intensity, radiated to upper back, unrelieved by Ibuprofen, aggravated by lying flat and associated with a frontal headache. He denied fever, weight loss, night sweats, cough or weakness. Vital signs revealed fever of 100.5F and pulse of 144 bpm. Physical exam revealed cachexia, lumbar paraspinal tenderness and cervical lymphadenopathy (LAD). Labs showed hemoglobin of 10 g/dl, WBC of 2.78 (4-11 K/uL), C-reactive protein 154.6 (< 5 mg/l), HIV viral load of 174 copies/ml and CD4 count of < 20/mm3. Alkaline phosphatase was normal. Chest X-ray and CT head were normal. He was started on antibiotics to cover for likely discitis/osteomyelitis and meningitis, and multi-modal analgesia. Lumbar puncture was done with normal opening pressure. Cerebrospinal fluid chemistry and microbiology were negative. Blood cultures and serum antigen for histoplasma, cryptococcus and toxoplasma were negative. MRI of the lumbar spine showed large retroperitoneal LAD and no evidence of infection. CT abdomen showed retroperitoneal LAD and hepatosplenomegaly. Excisional LN biopsy was done with pathology showing acid-fast bacilli with a negative Mycobacterium tuberculosis (TB) PCR. Presumptive diagnosis of disseminated mycobacterium avium complex (DMAC) was made and he commenced Azithromycin, Ethambutol and Rifabutin. Tissue and fungal blood cultures grew MAC 4 weeks later. His symptoms had markedly improved after 6 weeks of therapy.
Discussion: MAC is the most common nontuberculous mycobacterium in the context of AIDS. In the post-combined ART era, DMAC has become a rare diagnosis with an incidence of 2 events per 1000 patient years. (1) It remains a diagnostic challenge due to its non-specific presentation and delay in obtaining positive culture results. (2)DMAC usually presents with constitutional symptoms, LAD and hepatosplenomegaly. (1,2) While our patient did present with fever, his associated headache and back pain raised suspicion for an infectious cause prompting spinal imaging and CSF analysis, which were negative. Given diffuse LAD on imaging, tissue biopsy was warranted to rule out malignancy versus TB/MAC. The presence of AFB narrowed our differentials with PCR ruling out TB. MAC was later culture confirmed and the initiation of appropriate drug therapy resulted in symptomatic improvement.Our case highlights that DMAC can present with back pain due to severe retroperitoneal LAD and this LAD can thus be a useful clinical marker of response to treatment. (3) It also highlights the role of newer molecular techniques (eg. PCR) in aiding early diagnosis as culture results often lag.
Conclusions: DMAC has varied clinical presentations and should be included in the differential diagnosis of severe back pain in HIV/AIDS patients. Clinicians should have a low threshold for considering empiric treatment in high-risk patients (advanced AIDS) while awaiting confirmatory culture results.