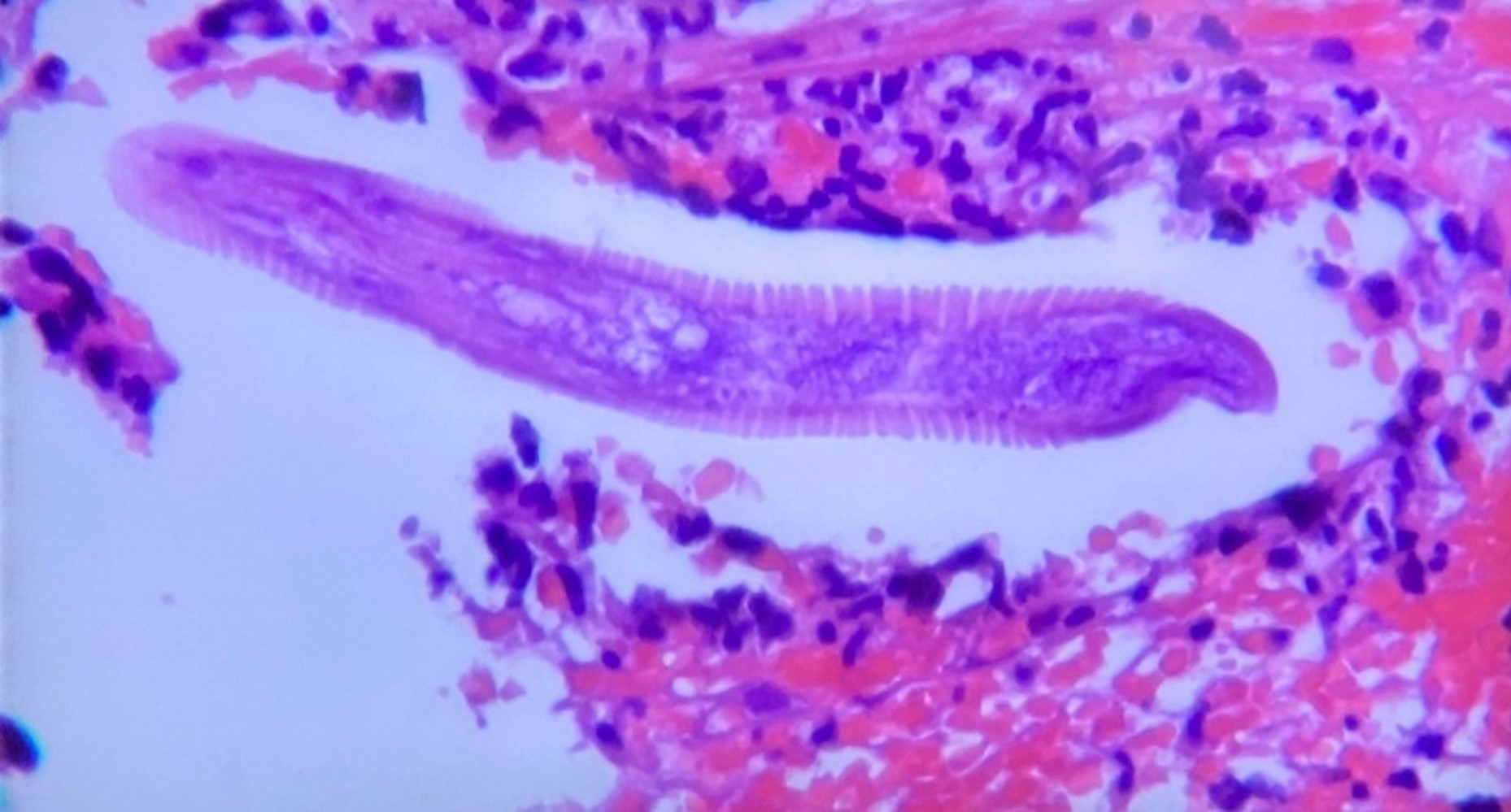
Case Presentation: A 63-year-old African American man with no past medical history, originally from the rural Pacific Coast in Colombia, South America, presented with two months of diffuse abdominal pain, intermittent diarrhea and dry cough. Other symptoms included low-grade fever and a 40-pound weight loss. He denied any rashes. Physical exam revealed a cachectic patient with pale conjunctivae, benign abdominal exam, no rash noted. Laboratory studies were relevant for a WBC 18,200 cells/uL, predominant neutrophils, normal eosinophil count, hemoglobin of 8.5 g/dL, albumin of 1.6 g/dL and negative HIV testing. CT abdomen and chest showed diffuse inflammatory changes of the small bowel wall, a right lower lobe consolidation and multiple pulmonary nodules. Blood cultures grew ESBL Klebsiella pneumoniae. Initial upper GI endoscopy and colonoscopy were normal. Due to uncertainty of diagnosis and concern for malignancy, an exploratory laparoscopy was done, showing distention of the proximal jejunum. Stool studies and biopsies revealed Rhabditiform larvae. Further testing was positive for HLTV-1 (Human T lymphotropic virus 1), concerning for disseminated infection. He was treated with Meropenem and Ivermectin with full recovery.
Discussion: Strongyloides stercoralis is estimated to infect 30-100 million people worldwide, especially those coming from tropical and subtropical areas (1). It usually presents as a chronic asymptomatic disease (1). In the immunosuppressed patient, hyper-infection or disseminated disease may occur (1). Definitive diagnosis of strongyloidiasis is made based on detection of larvae in the stool, sputum or duodenal fluid. However, strongyloidiasis is difficult to diagnose since the parasite load is low and the larval output is irregular in majority of the patients. The disease can be overlooked in non-endemic areas. Our patient presented with non-specific symptoms, but with significant weight loss concern for possible gastrointestinal malignancy. However initial work up was completed with an unclear diagnosis. His racial and geographical background and clinical presentation should raise concern for possible Strongyloides Stercoralis Hyperinfection Syndrome (SHS) and disseminated disease, even though our patient had no eosinophilia or rash. He was eventually found to have co-infection with HLTV-1, which is one of the most common risk factors for SHS (2). Patient in this group will have higher mortality associated with disseminated infection, and higher risk of developing HLTV-1 associated diseases, such as adult T-cell leukemia/lymphoma (2).
Conclusions: With increasing diversity in patient population, it is vital for internists to have a broader understanding of the epidemiology and background of patients, in order to have a high clinical suspicion for uncommon diseases.