Case Presentation:
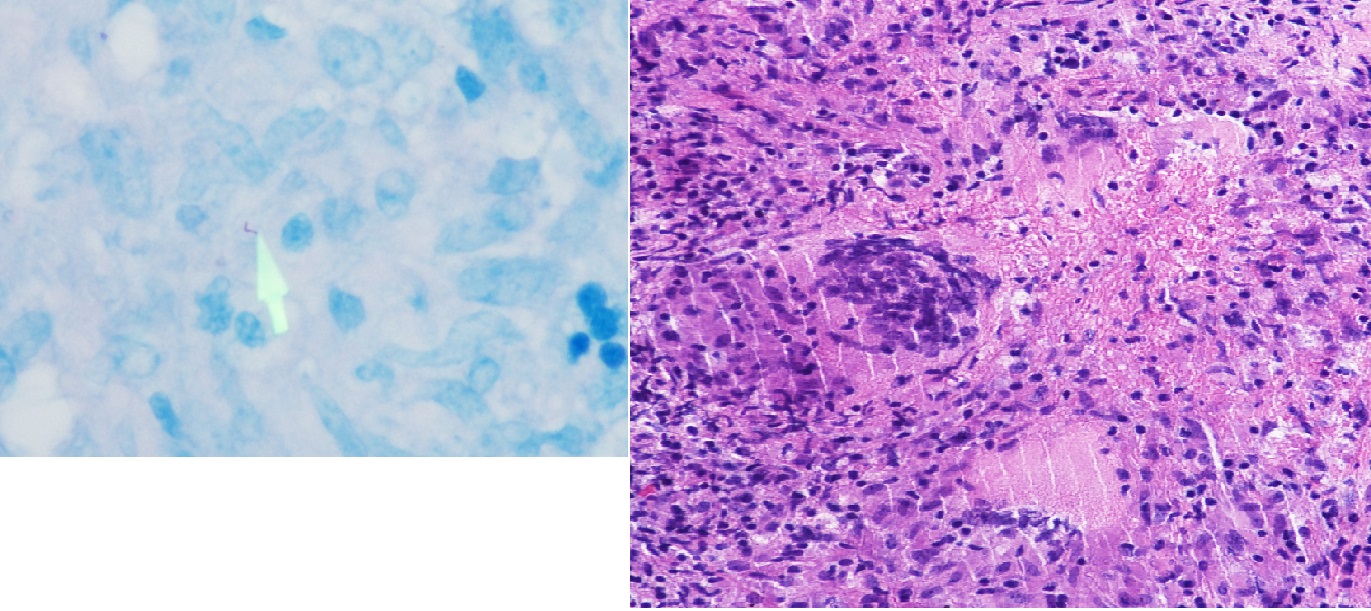
A 58 year-old man presented with a 3-month history of night sweats, chills and a 30 pound weight loss. His temperature was 102°F with decreased breath sounds and dullness to percussion at the left lung base. Labs were significant for a WBC 2.4 cells per µL with 22% monocytes and hemoglobin of 8.5 g/dl. CT of the chest with contrast revealed a right paratracheal lymph node mass measuring 4 x 5x 9 cm with a moderate left pleural effusion. FNA of the mediastinal lymph node and bone marrow biopsy were inconclusive. Quantiferon-TB Gold and HIV PCR were negative. A mediastinoscopy with tube thoracostomy was performed and pathology of the paratracheal lymph node revealed multiple caseating granulomas positive for AFB. Pleural fluid PCR was positive for Mycobacterium tuberculosis. A subsequent CT of the chest, abdomen and pelvis after surgery and 3 weeks after his initial presentation revealed new, innumerable punctate bilateral pulmonary nodules, abdominal lymphadenopathy and mesenteric infiltration consistent with disseminated TB. On detailed questioning the patient had no risk factors for TB exposure and denied history of frequent or opportunistic infections. The patient was started on isoniazid, rifampin, pyrazinamide and ethambutol with resolution of fevers within two weeks.
Discussion:
Isolated tuberculous mediastinal lymphadenopathy is extremely rare in an immunocompetent adult who had no apparent risk factors for tuberculosis. The differential diagnosis for isolated mediastinal lymphadenopathy includes sarcoidosis, malignancy, and infections including TB. The patient’s cytopenias and monocytosis were an initial clue that was consistent with disseminated TB. Eventually a subsequent CT showed disease progression to miliary tuberculosis, allowing us to see the natural history of this disease. This case also illustrates that tests for latent TB such Quantiferon-TB Gold cannot be relied upon to diagnose disseminated TB, as patients can test negative in up to 32% cases.
Conclusions:
TB should be included in the differential diagnosis of isolated mediastinal lymphadenopathy even in the absence of risk factors or immunosuppression. In cases of new mediastinal lymphadenopathy, if less invasive testing fails to provide a diagnosis, a hospitalist should pursue a mediastinoscopy as it often provides definitive diagnosis.