Background:
In a large tertiary‐care hospital, a quality improvement program was initiated to evaluate the current practices and trends in preoperative cardiac risk assessment and prescription of perioperative beta‐ers for patients undergoing elective, noncardiac surgery with a planned hospitalization ≥1 day.
Methods:
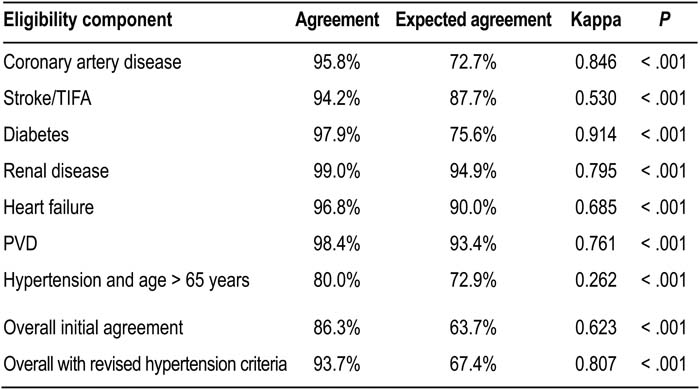
Data for this study originated exclusively from institutional databases, primarily the electronic medical record (EMR). Determinates of eligibility were defined using a standardized assessment and treatment protocol developed by a core working group of physicians, nurse‐practitioners, and pharmacists from the general internal medicine, anesthesia, cardiology, orthopedics, urology, colorectal surgery, vascular surgery, and general surgery departments. Clinical risk factors were assessed from documented diagnoses in the medical record. A validation sample (n = 190) of patients seen in 2005 was randomly generated from the analysis set of 11,985 consecutive patients. A single attending‐level physician reabstracted all relevant data for determining beta‐er eligibility from the validation sample. A kappa statistic was used to assess the rate of agreement between the original assessment and the validation assessment for determining beta‐er eligibility derived from the random sample.
Results:
The initial rate of agreement was moderate (kappa = 0.62). The rates of agreement for each eligibility component are indicated in the table. Closer examination revealed that characterization of hypertension had the lowest level of agreement. Originally, hypertension was defined by documented diagnoses in the electronic medical record, whereas the validation study used the actual measured blood pressure values. When the hypertension diagnosis was replaced with actual blood pressures (defined by the group as blood pressure > 160/90 mm Hg), the rate of agreement was substantially improved (kappa = 0.81).
Conclusions:
The content and quality of information in the EMR remains dependent in large part on the documentation practices of health care providers. EMR‐derived data can be used to produce valid correlates for quality improvement if they can be confidently validated with a random sample, as documented above. Clinically derived variables should be selected before diagnosis codes to define clinical conditions when it is feasible and when they are available to investigators.
Author Disclosure:
A. Aneja, None; E. Hixson, None; B. Harte, None; A. Jaffer, sanofi‐aventis, consulting fees or other remuneration (payment), speakers bureau; Astra‐Zeneca, consulting fees or other remuneration (payment); Society of Perioperative Assessment and Quality Improvement, nonremunerative positions of influence; Propmte, consulting fees or other remuneration (payment).