Background: Prescription opioids have come under increasing scrutiny in recent years due to the rise in use and misuse which has resulted in significant morbidity and mortality. There have been several efforts by government agencies to address this such as the FDA issuing a Risk Evaluation Mitigation Strategy (REMS) for extended release/long acting (ERLAs) opioids and the CDC issuing guidelines for prescribing opioids for chronic pain in 2016. However, these were only guidance for physicians and not mandated regulations. In 2017, the Commonwealth of Virginia passed legislation aimed specifically to address the opioid crisis prompting the State Board of Medicine to issue emergency regulations in March 2017 on the safe prescribing of opioids. Our objective was to examine how the regulations for Virginia physicians affected ERLAs prescribing patterns of physicians at the time of patient discharge from an 846-bed tertiary-care academic hospital.
Methods: We retrieved data on the daily ERLAs prescribed at the time of discharge from one year prior to the issuance of the regulations to one year after. Patients with sickle cell disease and those discharged from oncology and palliative care services were excluded. For each ERLA discharge prescription (dRx), we calculated morphine milligram equivalent (MME). We examined four outcomes: 1) number of ERLA dRx/day, 2) number of dRx/day/discharged patient, 3) total MME/day at the time of discharge, and 4) total MME/day/discharged patient. We used generalized linear models with log-link and gamma distribution due to marked right-skew of the all outcomes distributions. We used interaction between regulations and time-trend to determine the immediate effect of mandates and if regulations altered the subsequent time-trends of opiate prescriptions. This approach is consistent with interrupted time-series analysis assuming no lag-time effect.
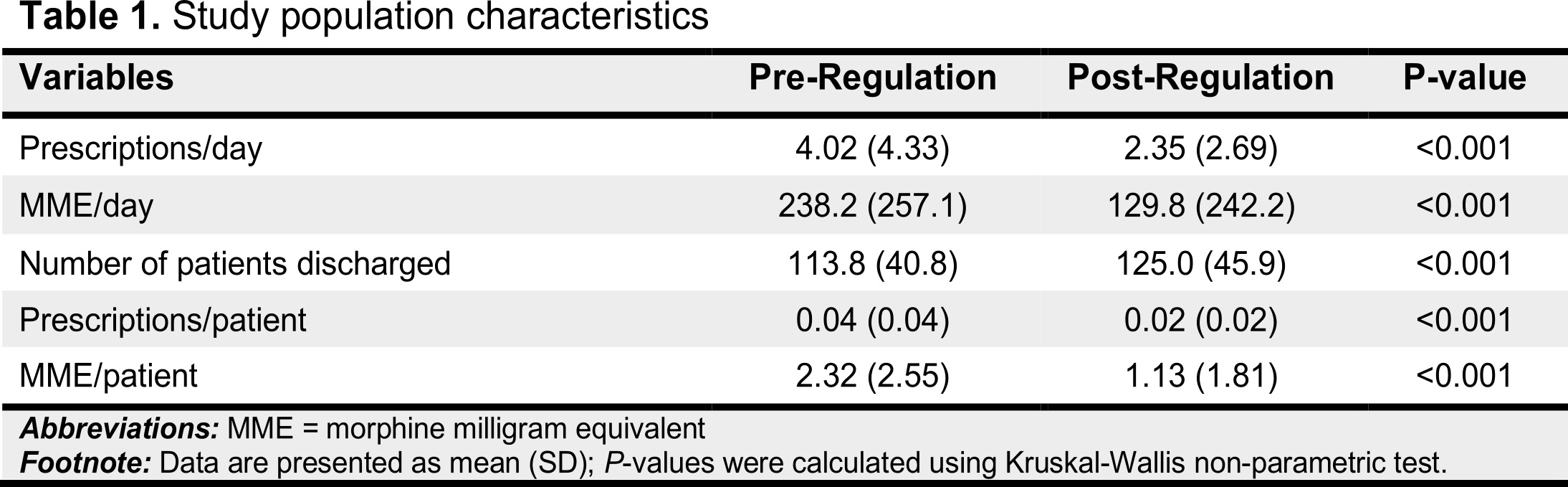
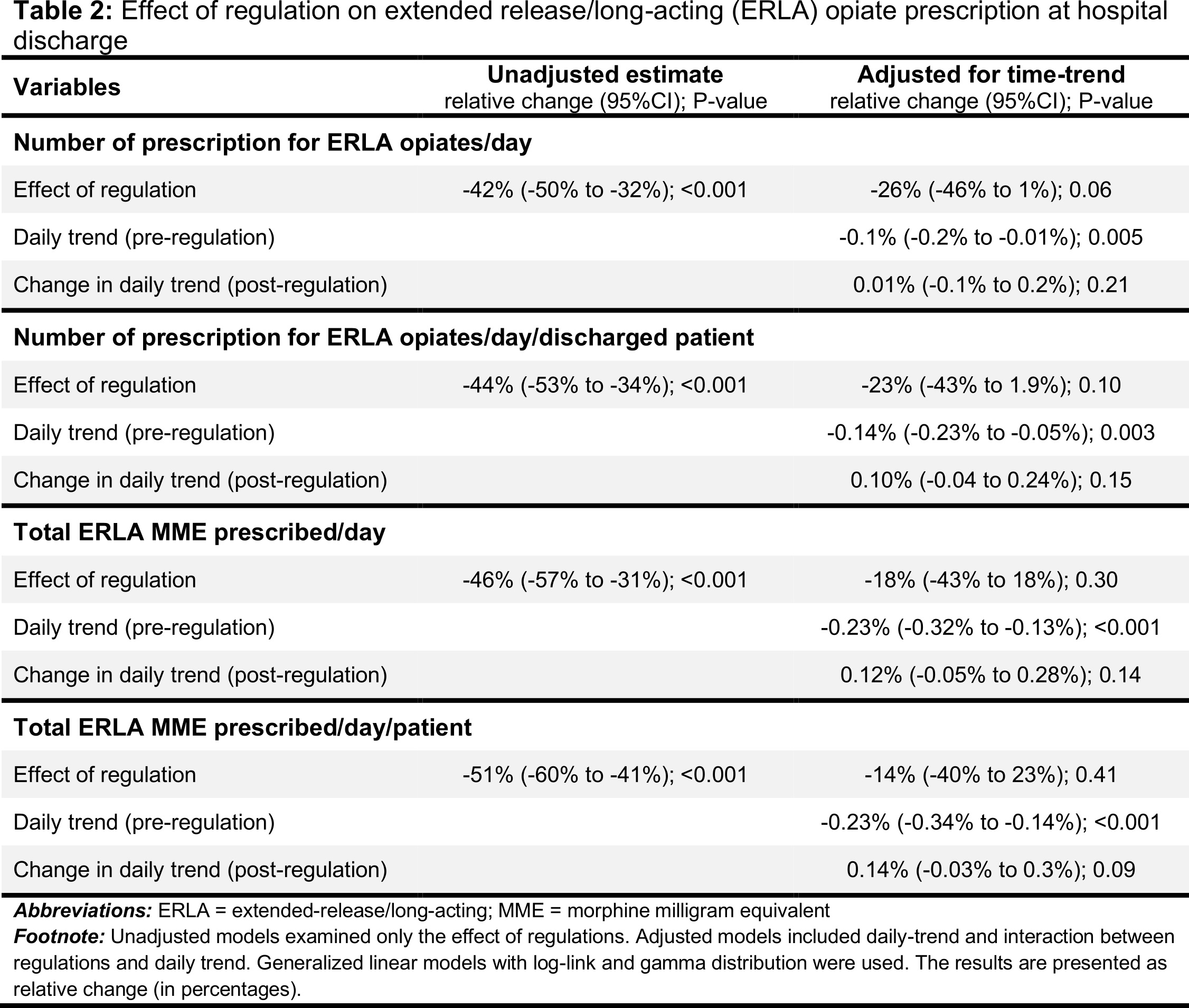
Results: Before the regulations, the mean (SD) number of ERLA dRx written was 4.0 (4.3)/day which decreased to 2.3 (2.7)/day after the regulations (difference = -1.7 Rx/day; P<0.001). Similarly, the amount of MME prescribed also decreased from 238.2 mg/day to 129.8 mg/day (difference = -108.4 mg/day; P<0.001). On the other hand, the number of patients discharged daily increased (113.8 to 125.0/day; P<0.001). There was a significant decreasing trend in the number of ERLA dRx written, number of dRx/patient, amount of MME/day, and amount of MME/day/patient, before the institution of regulations. Institution of regulations did not have an immediate effect nor did they change the subsequent time-trend of the dRx/day, dRx/day/patient, MEE/day, or MME/day/patient (Table 2).
Conclusions: The number and amount of ERLA prescribed at the time of discharge were decreasing before the institution of the Virginia Board of Medicine regulations. The regulations did not have a significant immediate or sustained effect on the prescribing patterns of discharging physician at a large teaching hospital. It is likely that the high level of awareness among physicians, before regulations went into effect, was effective in inducing the observed decline.